Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
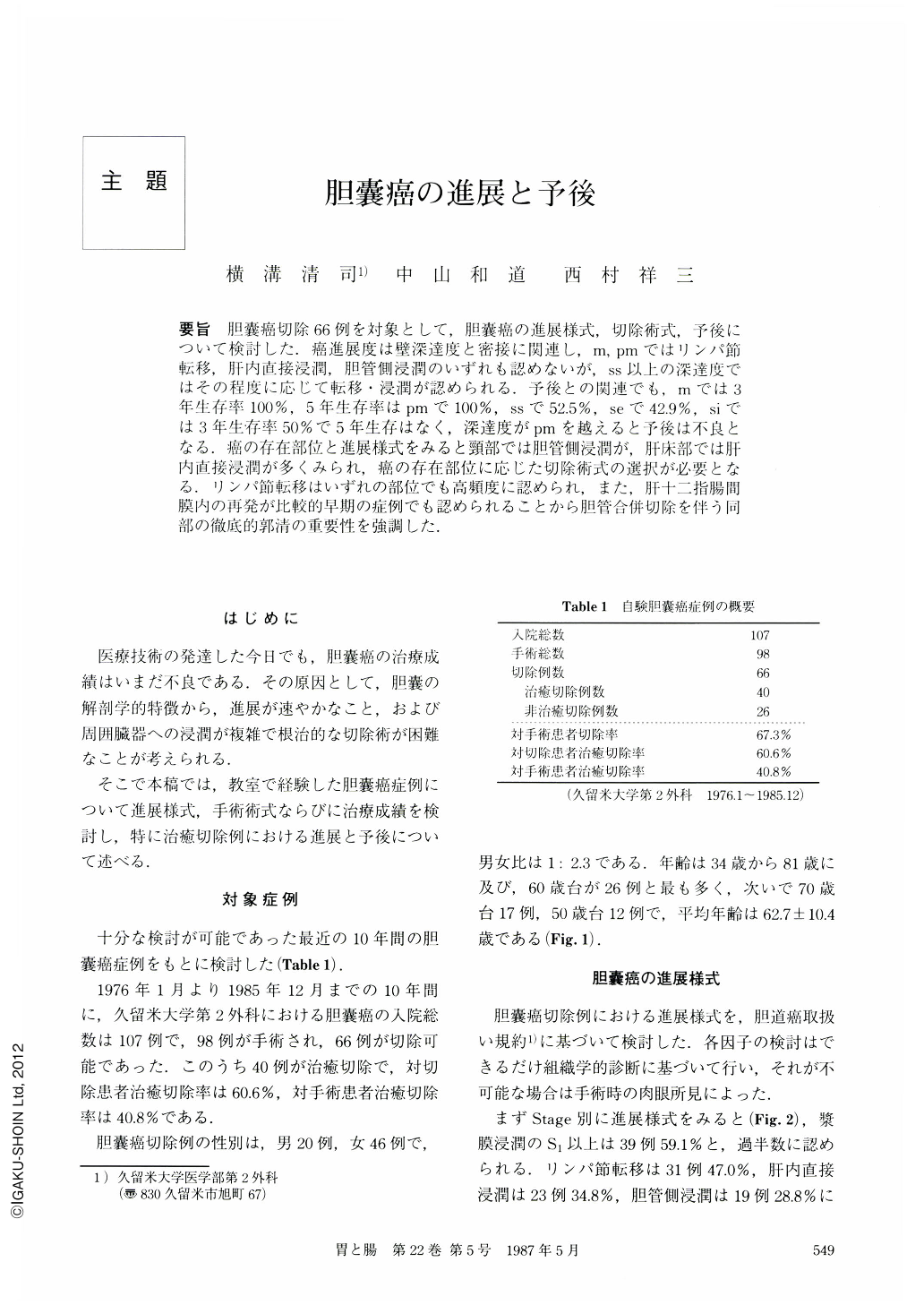
要旨 胆囊癌切除66例を対象として,胆囊癌の進展様式,切除術式,予後について検討した.癌進展度は壁深達度と密接に関連し,m,pmではリンパ節転移,肝内直接浸潤,胆管側浸潤のいずれも認めないが,ss以上の深達度ではその程度に応じて転移・浸潤が認められる.予後との関連でも,mでは3年生存率100%,5年生存率はpmで100%,ssで52.5%,seで42.9%,siでは3年生存率50%で5年生存はなく,深達度がpmを越えると予後は不良となる.癌の存在部位と進展様式をみると頸部では胆管側浸潤が,肝床部では肝内直接浸潤が多くみられ,癌の存在部位に応じた切除術式の選択が必要となる.リンパ節転移はいずれの部位でも高頻度に認められ,また,肝十二指腸間膜内の再発が比較的早期の症例でも認められることから胆管合併切除を伴う同部の徹底的郭清の重要性を強調した.
In 66 resected cases with carcinoma of the gallbladder, the extent of the spread of the carcinoma, operative procedure for resection, and the prognosis were studied. The spread of the tumors is closely related to the degree of the tumor invasion of the gallbladder wall. In the cases with tumors localized within the mucosa (“m”) and muscularis (“pm”), there was no metastasis to the lymph nodes nor direct invasion of the liver or the bile duct. However, in the cases with the tumors spreading beyond the subserosa (“ss”), there was metastasis and invasion related to the degree of spread. As to the relationship between the degree of invasion and its prognosis, there was a 100% chance of a three year survival rate in “m” and a 100% chance of a five year survival rate in “pm”, while there was a 52.5% chance of a five year survival rate in “ss”, a 42.9% chance of a five year survival rate in cases with tumors reaching as far as the serosa (“se”), and a 50% chance of a three year survival rate but no chance of survival beyond 5 years in cases with tumors infiltrating the serosa (“si”). The prognosis became worse when the invasion exceeded muscularis “pm”. As to the location of the carcinoma and its extension, the invasion of the bile duct from the lesion at the neck of the gallbladder, and the direct invasion of the liver from the lesion at the bed of the gallbladder were more frequently seen. Operative procedures should be selected in accordance with the location of the carcinoma. Metastasis most frequently seen from any location of the carcinoma was metastasis to the lymph nodes, and it was seen in the hepato-duodenal mesentery even a case of relatively early carcinoma which had been resected. Therefore, the importance of lymphadenectomy of the mesentery including cholecystectomy and resection of the bile duct was emphasized.
Copyright © 1987, Igaku-Shoin Ltd. All rights reserved.


