Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
はじめに
進行癌や,大きな潰瘍やポリープなどがX線診断の対象になっていた時代には,胃前壁病変のX線診断はあまり問題にならなかったようである.充盈法や粘膜法,圧迫法(現在のレベルの圧迫法ではない)で診断される病変が,そのままX線診断の限界と考えられていた,ところが,仰臥位の二重造影法によって胃後壁の早期癌が適確にX線診断されるようになり,次いで,胃カメラで胃前壁の早期癌(とくに表面陥凹型早期癌Ⅱc)がぼつぼつ発見されるようになったころから,胃前壁病変のX線診断はむずかしいと取沙汰されるようになった.仰臥位の二重造影法では適確に現わしえないからである.私どもが昭和40年に胃前壁の病変のX線診断には腹臥位二重造影法がよいことをはじめて報告したのはこの頃のことである.その後,腹臥位二重造影法は急速に普及し,多くの報告が発表された.工夫も加えられた.しかし,腹臥位二重造影法は,仰臥位の二重造影法に比べて,技術的にむずかしい,胃液の多いときにはよい写真がとれない.瀑状胃や肥満者では実施できないといったことから,どうものびなやみの感がある.
これとは別に,胃前壁病変とはいっても,隆起性病変か陥凹性病変かによって,病変の大きさや陥凹の差,存在部位,それに患者の個人差などによって,X線検査の仕方も当然変ってくる.また,病変を単にチェックするだけでよいのか,それとも精密検査をして病変を忠実に現わすことが必要なのかどうかによって,X線検査は違ってくる.
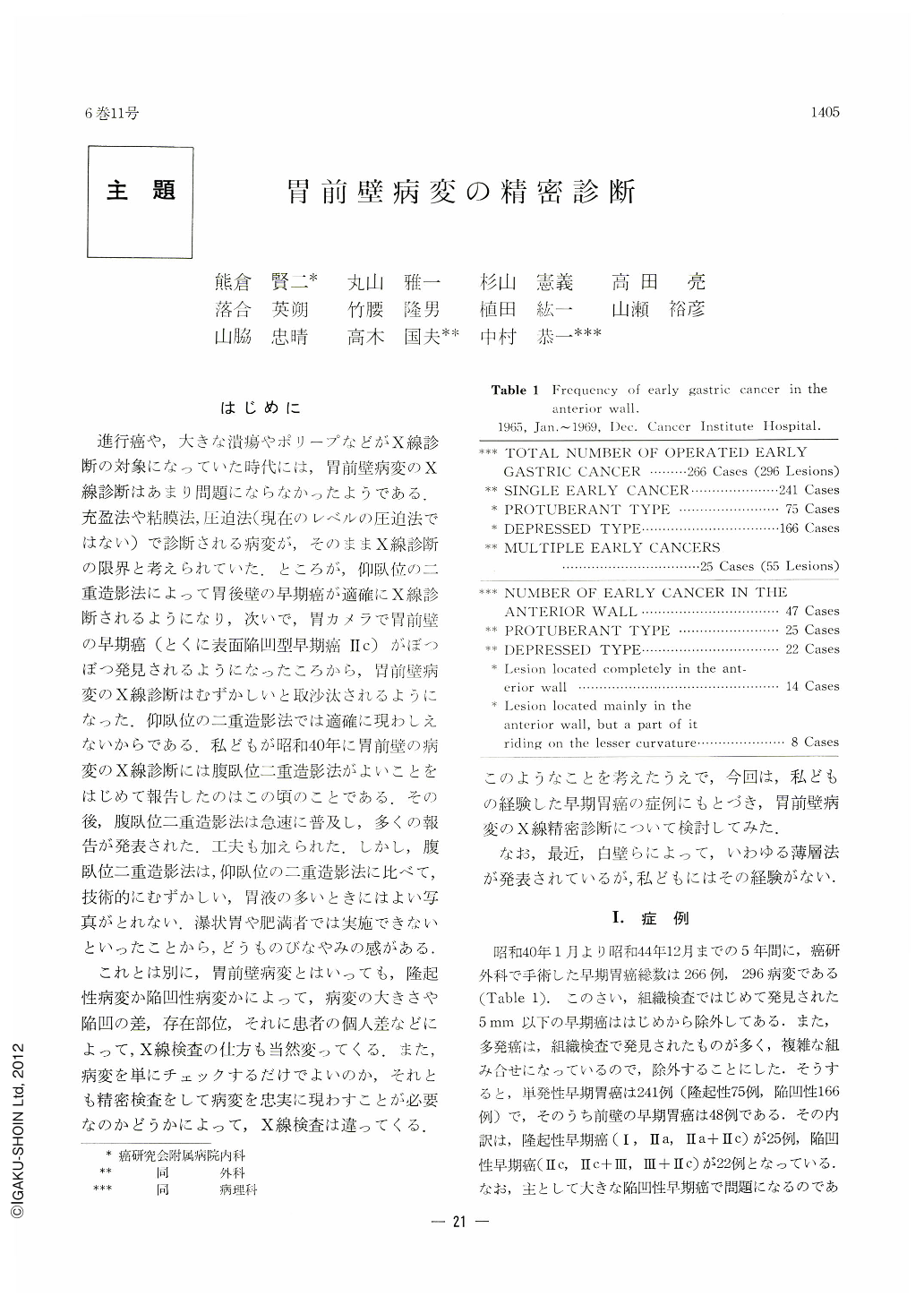
A series of 266 cases (296 lesions, excluding those less than 5mm in diameter discovered only by histology) of early cancer of the stomach have been experienced during the five-year period from January 1965 to December 1969 at Cancer Institute Hospital.
Of these, 241 cases were of single early cancer, including 75 of protuberant type and 166 of depressed variety, with 47 of them located on the anterior wall (25 of them protuberant and 22 depressed). An analysis was made of these 47 cases as to what kind of detailed examinations was performed for lesions on the anterior wall.
In 16 of 25 protruding lesions, compression revealed them most successfully (13 cases by compression in the upright and 8 likewise by it in the prone position).
As for the remaining 9 cases, (1) 5 were demonstrated to the best advantage by the double contrast method (3 in the supine and 2 in the prone); (2) 2 were lesions smaller than 10 mm (one a type Ⅱa, 7 mm in diameter, demonstrated in the prone mucosal relief picture with compression applied, and the other, a type Ⅱa, measuring 5mm in width, observed with some difficulty by upright compression); (3) and in the last 2 cases, their size was both so large that they were visualized by every examination in a way -but not too satisfactorily. After all, compression is the method of choice in demonstrating those smaller lesions, even when located on the anterior wall. The prone double contrast method is not always necessary in visualizing a lesion on this wall. It should also be remembered that an appropriate amount of air plays an important role in applying compression with success to a large lesion of type Ⅱa or Ⅱa+Ⅱc.
In 16 of 22 cases of depressed lesions, prone double contrast study proved best in demonstrating them. Of the remaining 6, (1) 2 of type Ⅲ+Ⅱc were best visualized by compression, (2) and in another 3, the whole aspects of the lesions were not seen to the best advantage by the prone double contrast method, but as such they were good enough for correct diagnosis; (3) and the last one was undetected in the same procedure, but was demonstrated by compression, although with difficulty. The prone double contrast method has, as it were, a blind spot.
There were five cases most faithfully demonstrated by comression (2 cases of type Ⅲ+Ⅱc and 3 type Ⅱc, both 20 to 30111111 in the greatest diameter with sharply outlined margin). However, too large a Ⅱc or Ⅱb-like lesion can not be visualized well by compression. There was also a case demonstrated most faithfully by prone mucosal relief picture.
The smallest lesion ever visualized faithfully by prone double contrast method measured only 6mm in diameter in a Ⅱc lesion and 15 mm in a Ⅱb-like lesion. After all, prone double contrast method, although technically complicated with afore-mentioned blind spot, is still the best procedure for the demonstration of the depressed lesion (especially Ⅱc) on the anterior wall.
Copyright © 1971, Igaku-Shoin Ltd. All rights reserved.


