Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
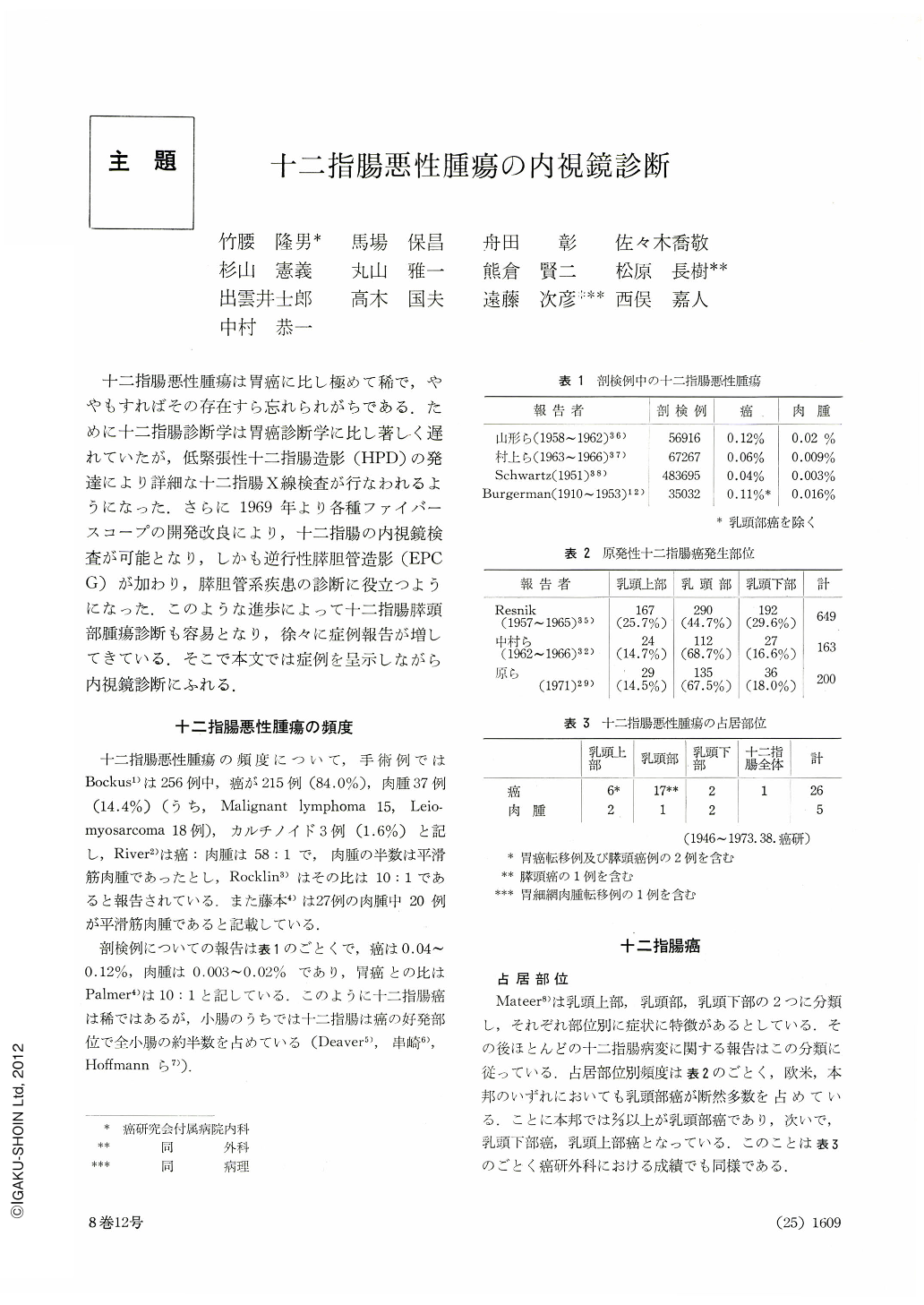
十二指腸悪性腫瘍は胃癌に比し極めて稀で,ややもすればその存在すら忘れられがちである.ために十二指腸診断学は胃癌診断学に比し著しく遅れていたが,低緊張性十二指腸造影(HPD)の発達により詳細な十二指腸X線検査が行なわれるようになった.さらに1969年より各種ファイバースコープの開発改良により,十二指腸の内視鏡検査が可能となり,しかも逆行性膵胆管造影(EPCG)が加わり,膵胆管系疾患の診断に役立つようになった.このような進歩によって十二指腸膵頭部腫瘍診断も容易となり,徐々に症例報告が増してきている.そこで本文では症例を呈示しながら内視鏡診断にふれる.
Malignant neoplasms of the duodenum are of greatly rarer occurrence as compared with cancer of the stomch. In autopsied cases the rate of duodenal cancer is said to be 0.04~0.12 per cent, and duodenal sarcoma 0.02~0.03 per cent. In surgically treated cases, the ratio of cancer versus sarcoma varies greatly according to reports, ranging from 6: 1 to 58: 1. Most of duodenal sarcomas are of leiomyosarcoma vareiety. the remaining few being malignant lymphoma.
During the period January 1946 to June 1973 the number of malignant tumors of the duodenum surgically managed at the Department of Surgery, Cancer Institute Hospital, totalled to 29: primary cancer in 24 cases and sarcoma in 5, including a case in which bulbar sarcoma was coexistent with reticulum cell sarcoma of the stomach. Thus cancer outweighed sarcoma with a ratio of 5: 1. According to Mateer's classification, the papillary region was the site of predilection: more than of frequency by cancer in the suprapapillary region and infrapapillary region, which was affected only in 2 out of 24 cases. Carcinoma of the ampullary region varies greatly in its designation. As cancer in this region arises from duodenal mucosa, pancreatic duct, common bile duct or pancreatic acinar duct, cancer developing from this area, aside from small one, makes it impossible to locate its site of origin. Consequently, excepting those cases in which their primary site had been clear from the outset, we included all cancers of this region in the group of papillary cancer. The name of cancer in the ampullary region seems dubious to us because the junction of the Vaterian bile duct and Vaterian pancreatic duct is not enlarged, and, furthermore, endoscopically this region is now generally called the longitudinal fold. As for macroscopical types of duodenal cancer, Borrmann types Ⅱ and Ⅲ predominated in the suprapapillary region, and type Ⅰ was seen in one case only. Conversely, in the papillary region cancer of Borrmann type Ⅰ was seen in 8 cases; type Ⅱ in 4, and type Ⅲ in 3 case. The tumor type was thus predominant here. In the infrapapillary region cancer of Borrmann types I and Ⅱ was seen each in one case. There was also seen a type Ⅳ cancer extending to all the portions of the duodenum. A single case of early papillary cancer localized within the mucosa was of tumor type. As for the relationship between the types according to the Borrmann's classification and lymph node metastasis and pancreatic infiltration, type Ⅰ was involved in 3/10; type Ⅱ in 3/7 and type Ⅲ in 2/4. Metastasis was thus more often seen in ulcerating type. It is quite natural that the size of a tumor is closely related with appearance of symptoms. The mean size of tumor in the suprapapillary region was 29×28 mm; that of the papillary region, 28×28 mm, and in the infrapapillary region it was 65×58 mm.
Histologically, all the cancer lesions belonged to tubule-froming varieties: adenocarcinoma tubulare or adenocarcinoma papillotubulare. Endoscopy was performed in 12 cases of duodenal cancer. Except for one case, all were of advanced carcinoma (including 2 cases of sarcoma). The rate of accurate diagnosis was 81 per cent. Endoscopic findings were almost similar to those of gastric cancer or colon cancer. Those in the supra- and infrapapillary regions showed ulceration of irregular shape accompanied with marginal embankment in addition to luminal stricture. In the papillary region the surface of Borrmann type Ⅰ was nodular with erosions and bleeding spots, while the surface of type Ⅱ and Ⅲ tumors was visualized as ulceration with marginal embankment centering on the papillary orifice. The margins of the ulcer were irregular and its floor was uneven. Endoscopic findings in the case of cancer in the papillary region such as swelling of the longitudinal fold, swollen papilla, bleeding spots, erosions, nodule formation and ulceration would undergo variegated changes according to enlargment of cancer.
Diagnosis by biopsy was accurate in 7/12 (60%). Atypical epithelium was seen in one case. In far advanced cancer cases, it was hard to grasp the whole picture of a given cancer. Sometimes we had to be content merely with gathering biopsical specimens from the mucosa around ulcer. For better results, more improved technique is desirable. In early carcinoma of the papillary region biopsical forceps must be inserted into the papillary orifice.
Two cases of duodenal sarcoma endoscopically observed were both of leiomyomsarcoma variety. When a central ulcer was formed on account of necrosis, diagnosis was made with ease, but when the tumor was seen as hemispherical protrusion with smooth surface, it was difficult to discriminate it from simple myoma. For correct diagnosis the size of the tumor must be duly taken into account as a factor in determining sarcoma.
Copyright © 1973, Igaku-Shoin Ltd. All rights reserved.


