Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
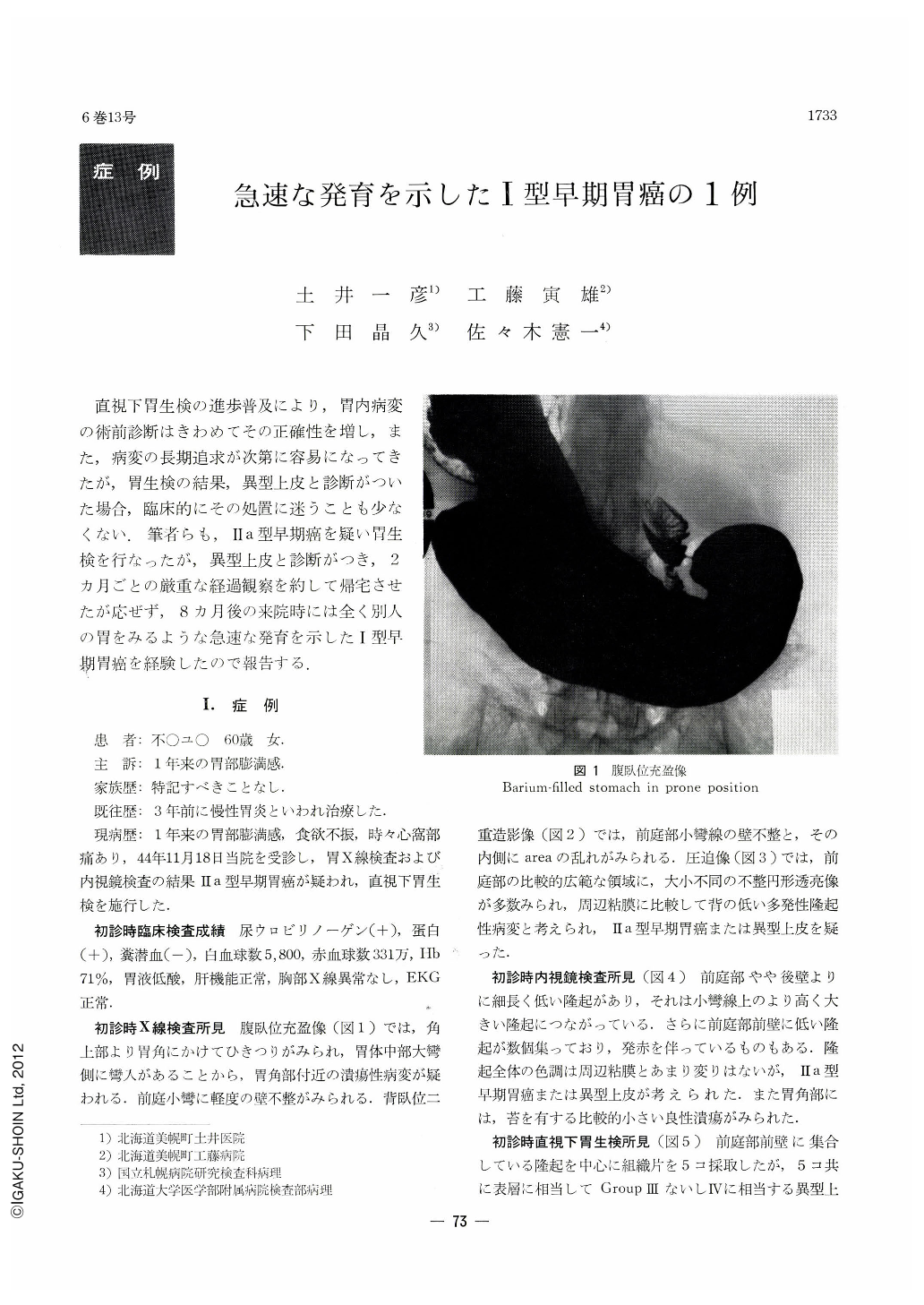
直視下胃生検の進歩普及により,胃内病変の術前診断はきわめてその正確性を増し,また,病変の長期追求が次第に容易になってきたが,胃生検の結果,異型上皮と診断がついた場合,臨床的にその処置に迷うことも少なくない.筆者らも,Ⅱa型早期癌を疑い胃生検を行なったが,異型上皮と診断がつき,2カ月ごとの厳重な経過観察を約して帰宅させたが応ぜず,8カ月後の来院時には全く別人の胃をみるような急速な発育を示した1型早期胃癌を経験したので報告する.
A 60-year-old female farmer had since one year before been complaining of full sensation in the stomach together with occasional epigastric pain. The initial x-ray and fibergastroscopic diagnosis made during the examination was type Ⅱ early gastric cancer or atypical epithelium (ATP) located from the lesser curvature of the antrum over to its anterior wall. The diagnosis by direct vision biopsy was ATP either of class Ⅲ or Ⅳ, but final diagnosis by histology was deferred to a later date. The patient was strictly asked to come for follow-up every two months, but she did not visit the authors' clinic until after eight months later. It was found then that the focus had developed in the interim to type Ⅰ early cancer or type Ⅰ (Borrmann) advanced cancer. Gastric biopsy also disclosed in all of the eleven histological specimens ATP of class Ⅲ or Ⅳ. As in all likelihood cancer focus could be found in a part of such a wide lesion, gastrectomy was performed.
In the resected stomach a broad-based irregular elevation was seen in the antrum, measuring 5.5×5.1×1.4 cm. Histopathologically, the surface epithelium of the lesion was mostly composed of ATP of class Ⅲ to Ⅳ, as had been seen at biopsy, but in some parts cancerous nests were seen here and there, including cells of adenocarcinoma mucocellulare in yet smaller parts. As minute cancer infiltration was also seen in the submucosa, the final diagnosis was type Ⅰ early gastric cancer with sm degree of invasion.
As has already been said, the gastric biopsy at the initial examination had confirmed this lesion as ATP of class Ⅲ or Ⅳ, and yet final diagnosis was deferred to a later date. However, when seen retrospectively, this lesion had in all probability been in the stage of type Ⅱ early cancer already at the time of initial examination, so that grave reflection is called for on the part of the examiner. The authors are now of the opinion that follow-up of ATP must be done in a comprehensive way: its size to be determined by x-ray, its nature by endoscopy and its histological diagnosis by biopsy. If followed up in this manner, other similar cases may possibly be found in an increasing number.
It also is of great interest to note that this lesion so rapidly grown mostly still shows morphological structure of ATP of class IV even at the time of resection. This fact seems to suggest that ATP of class IV should be regarded biologically as already in the stage of cancerized epithelium.
Copyright © 1971, Igaku-Shoin Ltd. All rights reserved.


