Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
抗生剤投与中に,腹鳴,腹痛,軟便,下痢などの下部消化器症状が少なからずみられるが,その大部分は投薬中止により速やかに改善する軽症例であり,臨床上重視されることは少なかった.しかし,ときに高熱,白血球増多を伴う激しい大腸炎症状を呈し,予後不良となる例のあることが古くから知られ,大腸を中心として広範な偽膜性の炎症所見を認めることから偽膜性腸炎と呼ばれてきた.
1950年代には,抗生剤投与により腸管内に黄色ブドウ球菌が異常増殖し,そのエンテロトキシンにより偽膜性腸炎が引き起こされると考えられていたが,1970年代末に至って,Clostridium difficile(C. difficile)の病原的意義が明らかにされ,抗生剤投与→C. difficileの異常増殖→毒素産生→偽膜性大腸炎発症,といった図式が描かれるようになった.この間の病因論についての目覚ましい進歩に対する興味はともかくとしても,抗生剤が多用される今日,本症の臨床的意義は大きい.偽膜性大腸炎は,しばしば発熱を伴うため,発熱の真の原因が抗生剤投与であることに気付かれぬまま,更に種々の抗生剤を投与し,大腸炎を一層悪化させている症例が散見されるからである.適切な診断,治療により,本症の大部分は治癒させることができるものであり,臨床家にとって本症に対する認識は不可欠のものと思われる.本稿では自験例を中心として,抗生剤投与による下痢症―偽膜性大腸炎におけるC. difficileの役割,臨床像,大腸内視鏡像,治療成績などについて述べることにする.
Pathogenic roles of Clostridium difficile, colonoscopic findings, clinical features and efficacy of oral vancomycin therapy were studied on antimicrobial agents associated diarrhea-pseudomembranous colitis in aged patients.
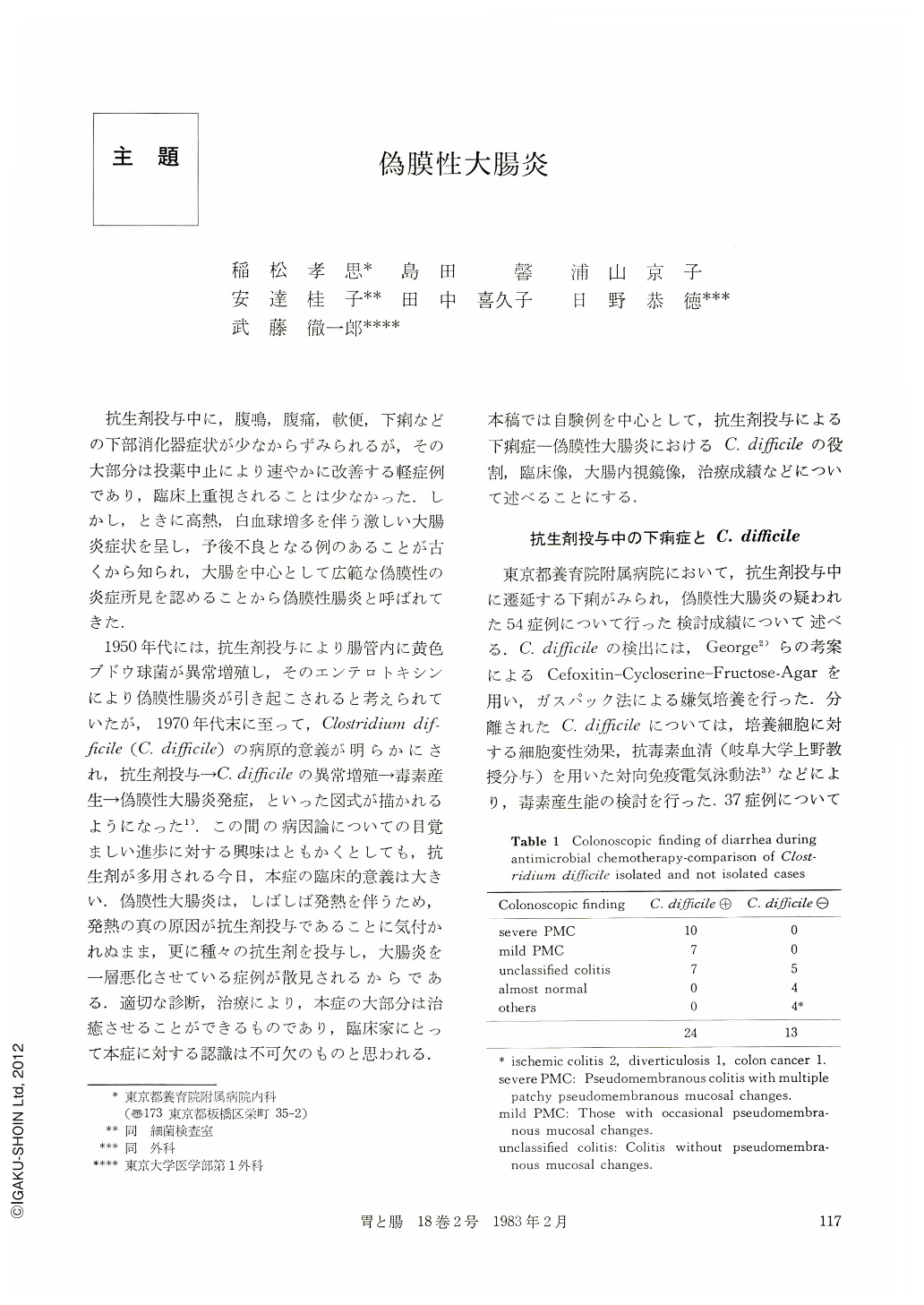
Clostridium difficile was isolated from 31 of 54 patients with antimicrobial agents associated diarrhea, and from all of 17 patients with pseudomembranous colitis confirmed by colonoscopic study. Colonoscopic findings of patients with Clostridium difficile isolation showed wide spectrum of inflammatory changes from multiple plaque-like pseudomembrane formation to minor redness and/or edema. Pseudomembranous colitis seems to be a severe form of colitis by toxinproducing Clostridium difficile.
Clinical features of 33 cases with pseudomembranous colitis which was confirmed by colonoscopy (22 cases) or autopsy (11 cases) were studied. Implicated antimicrobials were cephems, lincomycin, penicillins with broad spectrum, quinolincarbonates and rifampicin in 18, 11, 5, 2 and 1 patients respectively. One to 17 days after the start of causative antimicrobials, various frequency and quality of diarrhea occurred. Fever higher than 38℃, and leucocytosis more than 10,000/cmm were observed in 75.9% and 75.9% respectively. Hypoproteinemia (<5.5g/dl), hyponatremia (<137mEq/l) and hypokalemia (<3.3mEq/l) were observed in 65.5, 51.7 and 37.9% of cases respectively.
Eleven patients diagnosed by autopsy did not discontinue the implicated antimicrobials after the onset of diarrhea, and died on the fourth to 42th day. Thirteen patients diagnosed by endoscopy and treated without vancomycin recovered completely in 30.5 days on an average after the cessation of the implicated antimicrobials. Three of them died of underlying diseases or complications with resolution of colitis. On the other hand, nine patients treated with oral vancomycin recovered completely in 13.9 days on an average.
Copyright © 1983, Igaku-Shoin Ltd. All rights reserved.


