Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
クローン病は1932年Crohnら1)によって,回盲部結核とは異なる新しい臨床的,病理学的疾患単位としてregional ileitisの名称で報告されたものであるが,その後回腸末端部ばかりでなく,大腸(Colp2),1934;Crohn and Rosenak3,1936)およびその他の消化管にも病変のある症例が報告されるに至り,regional enteritisまたはCrohn's diseaseと称されるようになっている.一方,クローン病に似た肉芽腫性病変が大腸だけにみられる場合については,大腸の原因不明の非特異性炎症である潰瘍性大腸炎との異同が問題となるので,1950年代まで潰瘍性大腸炎に含めて扱われていた.しかるに,近年,クローン病に似た肉芽腫性病変を示す大腸炎の多くは,臨床的,病理学的所見を総合すれば潰瘍性大腸炎と区別できることが明らかにされ,Colonic form of Crohn's disease(Wells4),1952),Crohn's colitis(Brooke5),1959),Crohn's disease(regional enteritis)of the large intestine(Lockhart-Mummery and Morson6),1960),Granulomatous colitis(Wolf and Marshak7),1962)などと呼ばれ,ことに1968年のプラハでの国際消化器病学会議以来Crohn's disease of the colonと称されている8).なおこれらはCIOMSの国際用語集9)ではregional colitisと呼ぶこととなっている.
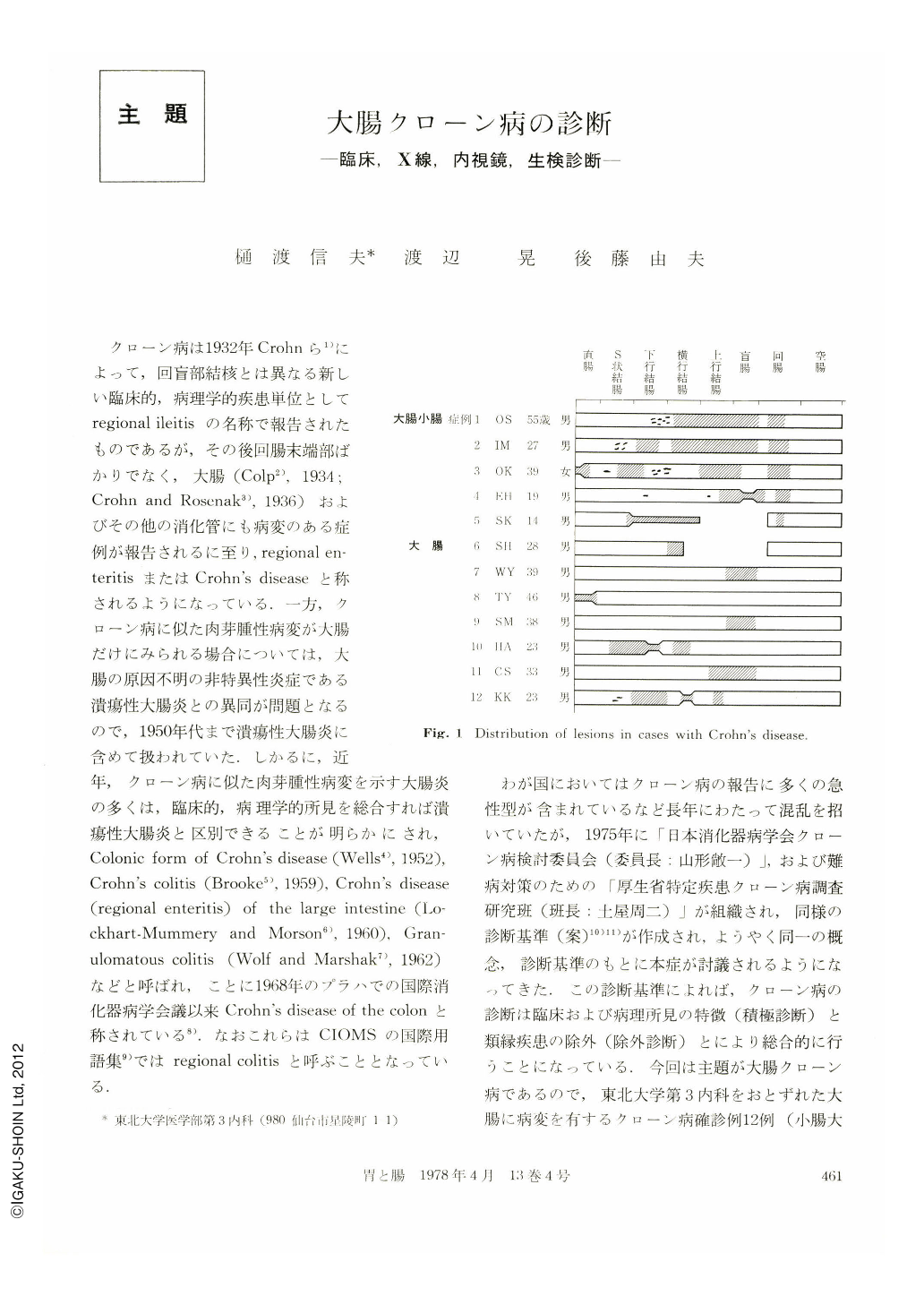
わが国においてはクローン病の報告に多くの急性型が含まれているなど長年にわたって混乱を招いていたが,1975年に「日本消化器病学会クローン病検討委員会(委員長;山形敞一)」,および難病対策のための「厚生省特定疾患クローン病調査研究班(班長:土屋周二)」が組織され,同様の診断基準(案)10)11)が作成され,ようやく同一の概念,診断基準のもとに本症が討議されるようになってきた.この診断基準によれば,クローン病の診断は臨床および病理所見の特徴(積極診断)と類縁疾患の除外(除外診断)とにより総合的に行うことになっている.今回は主題が大腸クローン病であるので,東北大学第3内科をおとずれた大腸に病変を有するクローン病確診例12例(小腸大腸クローン病5例,大腸クローン病7例)(Fig.1)の成績を中心に内科の立場での積極診断,つまり症状,臨床検査所見,X線所見,内視鏡所見,生検所見における本症の特徴と,除外診断としてはわが国ではもっとも問題である腸結核との鑑別について述べてみたい.
Twelve cases of Crohn's disease involving the large bowel (5 involved both small and large bowel and 7 only large bowel) are studied with special reference to the characteristics on clinical signs, laboratory data, X-ray findings, endoscopic findings and histologic findings of biopsy material.
Following conclusions were obtained in the comparative study with intestinal tuberculosis.
1. Abdominal pain, diarrhea, loss of body weight, fever and abdominal tumor were common in both diseases, but bloody stools, external fistula and anal lesion were characteristic of Crohn's disease.
2. The tuberculin test was negative in most cases of Crohn's disease, but positive in almost all cases of intestinal tuberculosis. The demonstration of tubercle bacilli from feces and biopsy tissues of lesions was difficult in the latter.
3. In X-ray findings and endoscopic findings discontinuous or segmental lesion associated with stenosis was seen in both diseases. The cobblestone appearance, gyrous lesions. longitudinal ulcers in the small bowel, fissures and fistulae were chracteristic of Crohn's disease. On the other hand, scarred area, pseudopolyposis, irregular undermined ulcers, circular ulcers were characteristic features of tuberculous lesion.
4. Granulomas were frequently observed in biopsy material of both diseases. However, recognition of caseous necrosis was almost impossible even in tuberculous lesion. Granulomas of the mucosa even in tuberculosis were solitary and small and very difficult to differentiate from those in Crohn's disease. On the other hand, “disproportional inflammation”, normal mucosa intervening in the lesions and neuromatous hyperplasia in the submucosa were frequently observed in Crohn's disease.
5. If the above mentioned differential points are applied, the clinical differential diagnosis in typical cases appears to be definitely possible.
Since the demonstration of tubercle bacilli or caseous necrosis in the tissue is difficult, therapeutic differential diagnosis with antituberculous therapy should be used in atypical cases.
Copyright © 1978, Igaku-Shoin Ltd. All rights reserved.


