Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
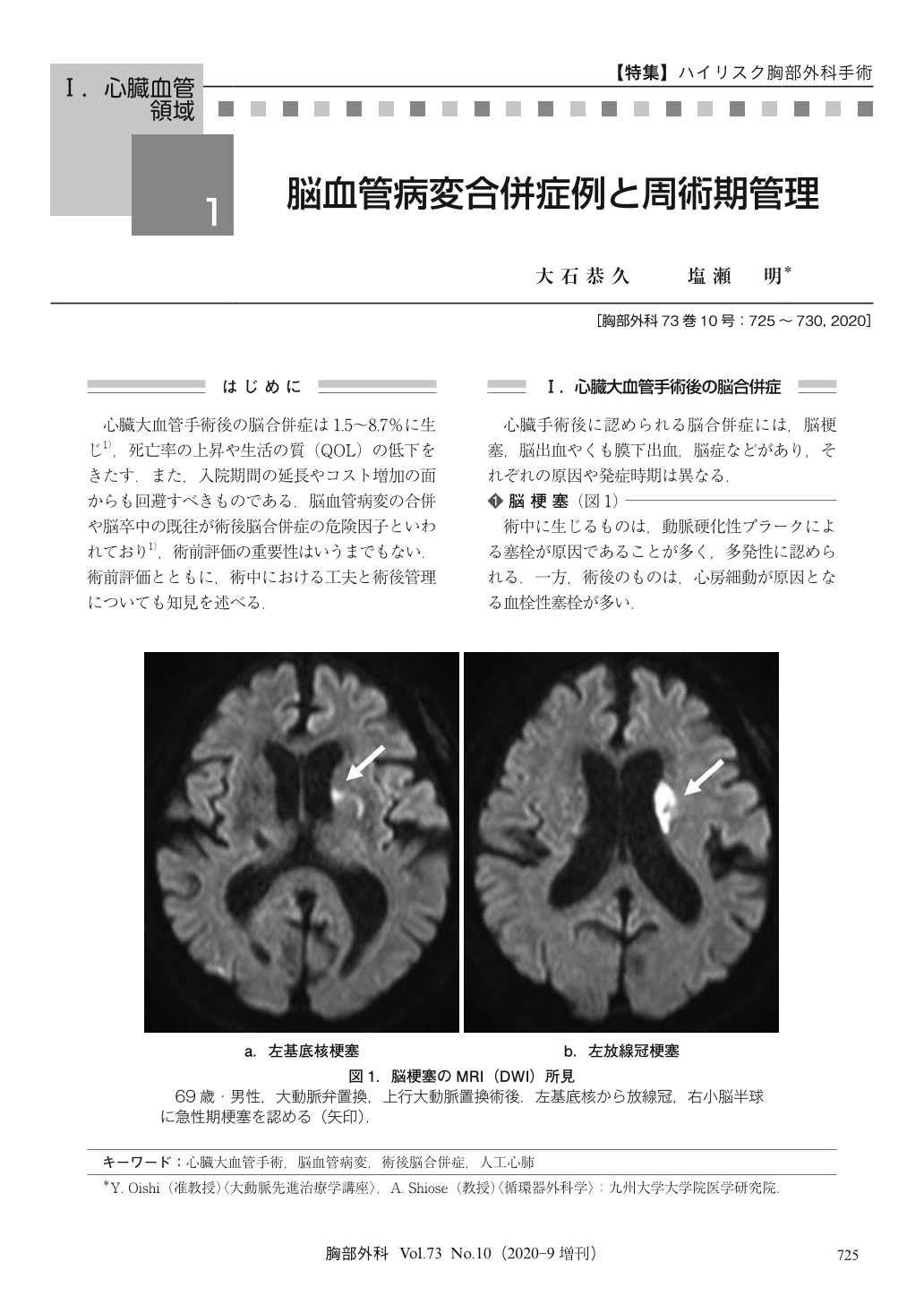
心臓大血管手術後の脳合併症は1.5~8.7%に生じ1),死亡率の上昇や生活の質(QOL)の低下をきたす.また,入院期間の延長やコスト増加の面からも回避すべきものである.脳血管病変の合併や脳卒中の既往が術後脳合併症の危険因子といわれており1),術前評価の重要性はいうまでもない.術前評価とともに,術中における工夫と術後管理についても知見を述べる.
Stroke is an important cause of morbidity and mortality after cardiovascular surgery and its incidence has been reported as 1.5 to 8.7%. Preexisting cerebrovasuclar disease, stenotic lesions of the carotid artery and atherosclerosis of the ascending aorta are known to be significant anatomic risk factors. To prevent perioperative stroke, it is important to discuss the onset mechanisms. Intraoperative stroke is mainly caused by the embolization of scattered atheroscrelotic plaque. Carotid duplex scanning and magnetic resonance imaging (MRI) are useful methods for the preoperative screening of cerebrovascular stenosis and plaque. Enhanced computed tomography (CT) is a powerful tool to estimate the presence of severe atheroscrelotic plaque in the aorta. When severe plaque is present, the manipulation, cannulation or clamping of the diseased aortic segment should be prevented. Insufficient oxygenated brain blood flow is thought to be another mechanism of intraoperative stroke. Impaired cerebral autoregulation during caridopulmonary bypass has been reported. Thus, it is recommended to maintain a high mean arterial pressure during cardiopulmonary bypass, especially in patients with cerebrovasuclar occlusive diseases. Postoperative stroke is mainly caused by embolization of the thrombus. To prevent this, excessive hypovolemia and atrial fibrillation should be avoided. Preemptive usage of beta blockers is one option for preventing postoperative atrial fibrillation.
© Nankodo Co., Ltd., 2020


