Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
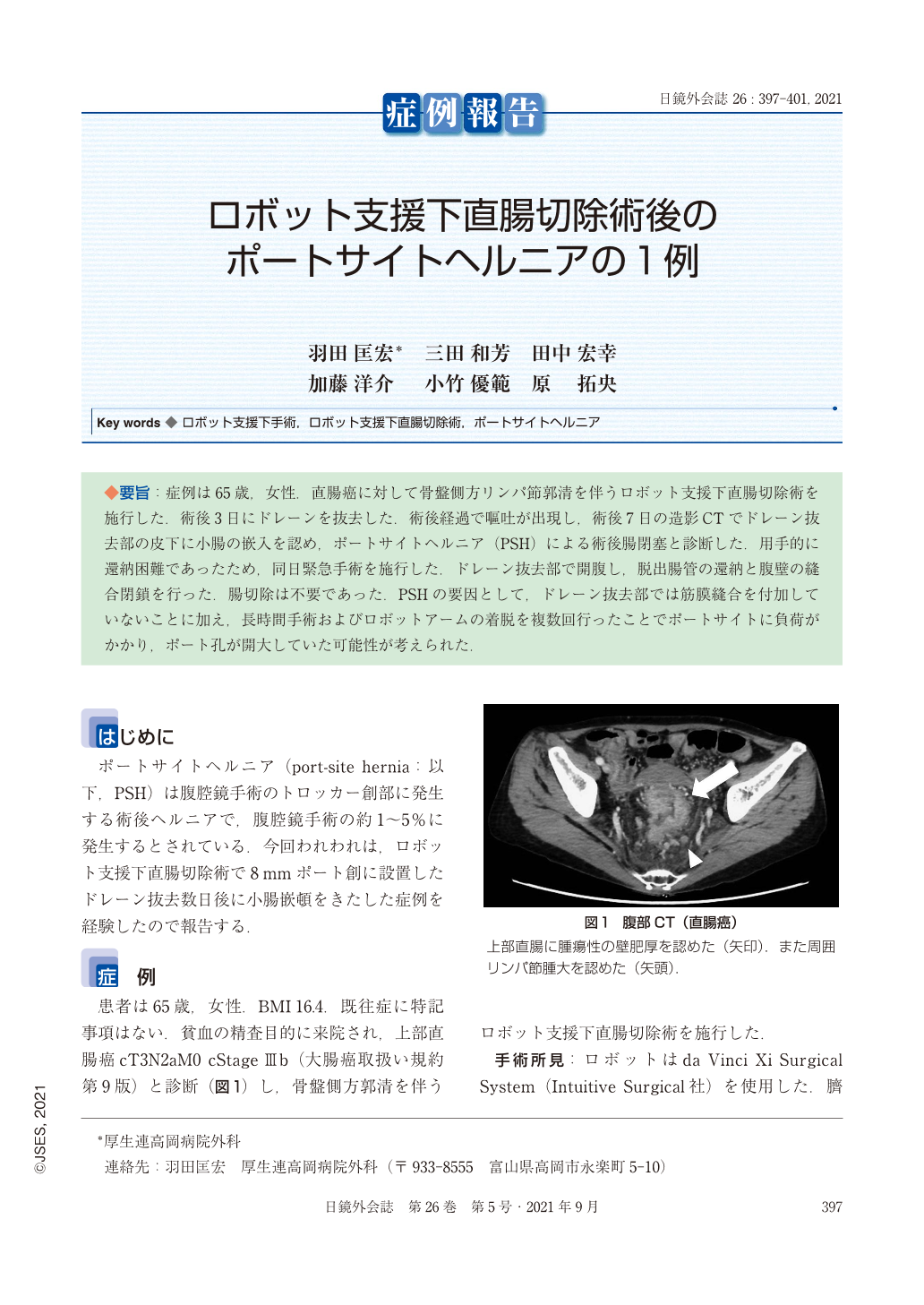
◆要旨:症例は65歳,女性.直腸癌に対して骨盤側方リンパ節郭清を伴うロボット支援下直腸切除術を施行した.術後3日にドレーンを抜去した.術後経過で嘔吐が出現し,術後7日の造影CTでドレーン抜去部の皮下に小腸の嵌入を認め,ポートサイトヘルニア(PSH)による術後腸閉塞と診断した.用手的に還納困難であったため,同日緊急手術を施行した.ドレーン抜去部で開腹し,脱出腸管の還納と腹壁の縫合閉鎖を行った.腸切除は不要であった.PSHの要因として,ドレーン抜去部では筋膜縫合を付加していないことに加え,長時間手術およびロボットアームの着脱を複数回行ったことでポートサイトに負荷がかかり,ポート孔が開大していた可能性が考えられた.
A 65-year-old woman underwent robot-assisted rectal resection for rectal cancer. A drain was withdrawn on the third postoperative day. Vomiting appeared on the fifth postoperative day. Abdominal computed tomography (CT) showed bowel obstruction due to incarceration of the small intestine at the site of the 8-mm port without drainage tube in the upper right abdomen. An urgent operation with a diagnosis of port site hernia (PSH) was performed. After the aponeurosis was opened, a strangulated small intestine was observed in the free space under the aponeurosis.
It was concluded that one of the factor of PSH was long surgery time, the port site was damaged by performing robot docking multiple times, and suturing of all abdominal wall layers including the peritoneum was necessary at the time of port site closure.
Copyright © 2021, JAPAN SOCIETY FOR ENDOSCOPIC SURGERY All rights reserved.