Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
硬膜動静脈瘻の頭蓋内出血のrisk factorとしてのcortical venous drainageはよく知られているが1-3,5-8,11),海綿静脈洞部硬膜動静脈瘻で頭蓋内出血をおこす頻度は比較的稀とされている1,5).今回,われわれは鉤静脈を介して嗅静脈へ流出するcortical venous drainageよりの脳内出血と思われる所見を呈し,経静脈的塞栓術中にも同じ部位へのextravasationを来たした症例を経験した.硬膜動静脈瘻におけるcortical venous drainageの意義,及び経静脈的塞栓術を行うにあたり,cortical venous drainageをまず塞栓することが肝要であることの重要性を改めて認識したので文献的考察を加えて報告する.
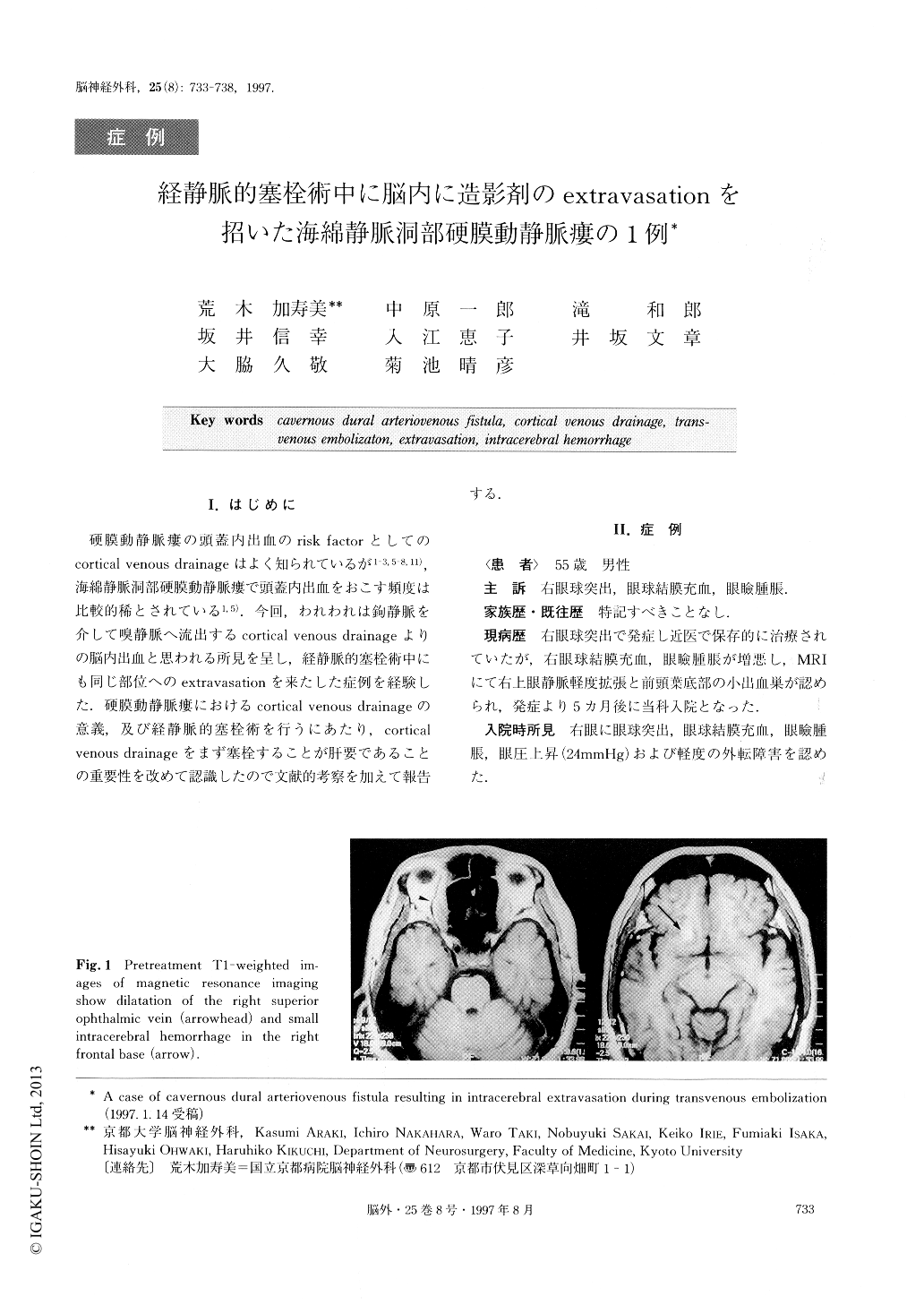
Cortical venous drainage has been described as one of the major risk factors for dural arteriovenous fistula, which may induce venous hypertension leading to venous ischemia or intracerebral hemorrhage. However, it is rather rare to observe cortical venous drainage manifesting in this way in the cavernous sinus region. We report a case of a 55-year-old gentleman with a right cavernous dural arteriovenous fistula, presenting with conjunctival chemosis, exophthalmus and ocular hypertension on the affected side. Magnetic resonance imaging showed a small intracerebral hemorrhage in the right frontal lobe. Cerebral angiography revealed a dural arteriovenous fistula in the right cavernous sinus draining into the right olfactory vein via the uncal vein, as well as into the superior and inferior ophthalmic veins. This unusal cortical venous reflux was thought to be consistent with the intracerebral hemorrhage found on the magnetic resonance imaging.
The patient underwent transvenous embolization for the dural arteriovenous fistula using an inferior petrosal sinus approach. Obliteration of the superior and inferior ophthalmic veins was performed first because selective catheterization into the uncal vein was difficult, and the cortical venous reflux through the vein seemed to be slight. However, extravasation of the contrast material occurred in the right frontal lobe after obliteration of the ophthalmic veins during the procedure. The cause of the extravasation was suspected to be the same olfactory vein that had been involved in the previous intracerebral hemorrhage. The obliteration of the dural fistula was continued rapidly, and the fistula dis-appeared after the embolization. Neurologically, the pa-tient had no noticeable troubles, except for a mild head-ache. The pretreatment symptoms were alleviated with-in several days, and the patient was discharged in a week.
We emphasize the following points from this rare case in order to facilitate a safer procedure during transvenous embolization for cavernous dural arteriove-nous fistula. It is important to obliterate the cortical venous drainage as early as possible, even if the reflux is small or the catheterization is difficult. Repeated, careful sinography is useful for the evaluation of the drainage pattern at certain stages during the trans-venous embolization procedure.
Copyright © 1997, Igaku-Shoin Ltd. All rights reserved.


