Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
下垂体腺腫の中でprolactinomaはbromocriptine(BC)投与により血中prolactin(PRL)濃度の低下と腫瘍の縮小が期待できることが知られている6,13,19,20).BC療法の合併症については種々の報告があるが,その一つとして髄液漏がある.これはprolactinomaがしばしば骨を含めた周辺組織の破壊を伴って発育するため,BC投与により腫瘍が縮小し,蝶形骨洞,乳突洞などに髄液の流出路が開き,髄液鼻漏や髄液耳漏が出現すると考えられている1,2)。しかしこれまでに髄液鼻漏1-3)と髄液耳漏4)についての報告は少数みられるだけであり,特に後者は極めて稀である.
最近われわれはBC療法中,髄液鼻漏と髄液耳漏が出現し,経蝶形骨洞手術と腰椎ドレナージにより治癒した巨大なprolactinomaの1症例を経験したので,その機序について若干の文献的考察を加えて報告する.
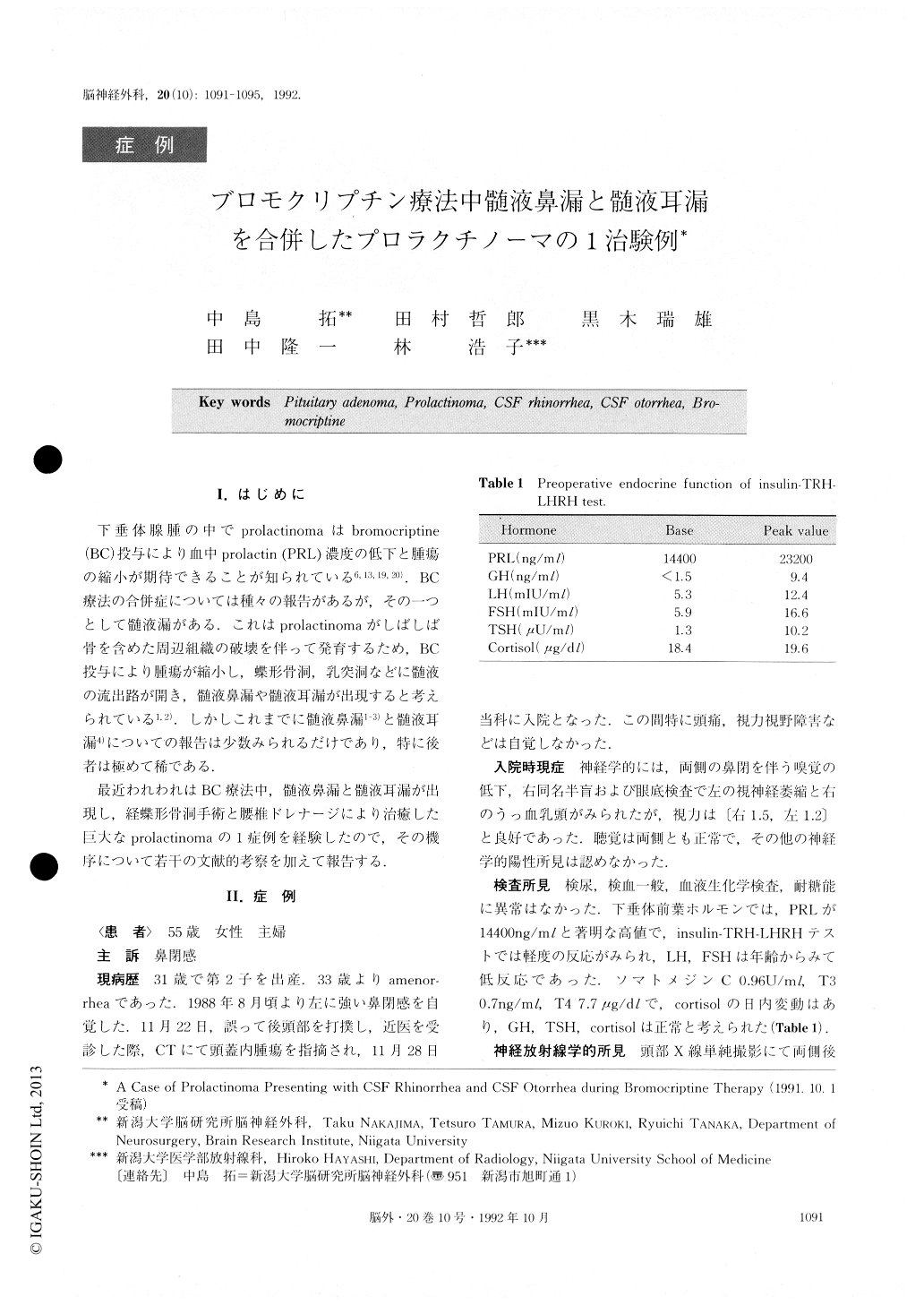
Cerebrospinal fiuid (CSF) leakage is a rare complica-tion of prolactinoma treated with bromocriptine (BC).BC is known to be effective for reducing the volume of aprolactinoma and fordecreasing the serum level of pro-lactin (PRL). In cases of pituitary tumors, CSF leakage isthought to be caused by shunting between the subarach-noid and extradural spaces. We had a case presentingwith CSF rhinorrhea and CSF otorrhea during BC ther-apy which was treated successfully, The mechanism andtreatment of CSF leakage were studied.
A 55-year-old woman complaining of nasal obstruction and headache was admitted to our hospital on Nov. 22, 1988. CT scan showed a huge intracranial mass lesion in-volving the sella and the supra-sellar region and invading the sphenoid sinus and ethmoid sinus. Serum YRI. level was 18,000 ng/mi "I'he patient was diagnosed as having an invasive prolactinoma, and BC therapy (5.0 mg per (lay) was instituted. Three days later, CSF rhinorrhea de-veloped, and BC treatment discontinued ; radiation ther-apy was started- After :31i ('y irradiation the size of the tumor was same on (°1 , and serum level of PRI, was still high. The patient underwent trans-sphenoidal operation. The tumor was removed partially and the presumed ('SF fistula was repaired. The sella and sphenoid sinus were packed with fat. BC treatment was reinstituted, and the serum I RI. level decreased gradually without recurrent CSF rhinorrhea. Two weeks later the patient returned complaining of bilateral hearing disturbance. With a dia-gnosis of exudative otitis media she underwent bilateral tympanostomy. Immediately after tympanostomy, pul-sating discharge from the middle ear was observed. The continuous discharge was serous, clear and glucose-positive. On CT scan, mastoid air cells and the middle ear bilaterally were of water density. A diagnosis of CSF otorrhea was made, and lumbar spinal drainage was started. Five clays later the CSF otorrhea stopped, even with removal of the lumbar drain. Ten clays later the pa-tient was discharged without headache or liquorrhea, although bilateral hearing disturbance remained ; serum PRI_ level was normal.
Few cases of prolactinoma presenting with CSF rhi-norrhea during BC therapy have been reported. Reports of CSF otorrhea during BC therapy are even rarer, and we could not find any case presenting with both of rhi-norrhea and otorrhea at the same time. In our case, CSF leakage was associated with extradural extension of tumor. CT scanning showed the tumor invasing to sphe-noid sinus, posterior ethmoid sinus and the edge of pyra-mis bilaterally. With decrease in tumor volume following BC therapy, a CSF pathway might have been opened. Fluid in pyramis or mastoid air cells usually does not produce otorrhea. It is possible that obstruction of the Eustachian tube accompanied a CSF leakage and that CSF remaining in the middle ear drained externally after tympanostomy. Trans-sphenoid operation was thought to be the most effective treatment for repairing the CSF rhinorrhea. Operative treatment had been recommended for CSF otorrhea as well, but our case was treated with spinal drainage. The patient has remained neurologically stable for the past two years.
Copyright © 1992, Igaku-Shoin Ltd. All rights reserved.


