Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
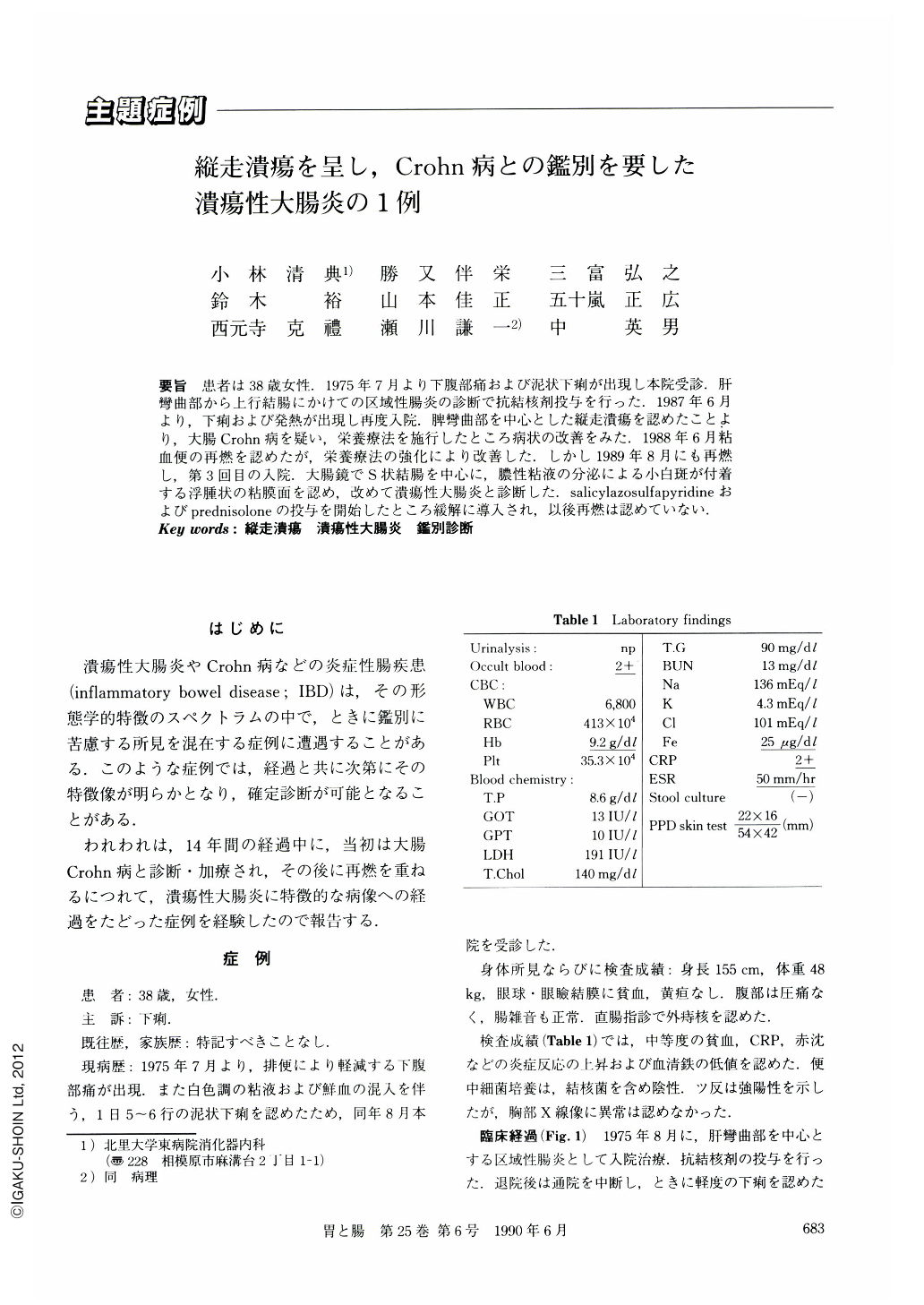
要旨 患者は38歳女性.1975年7月より下腹部痛および泥状下痢が出現し本院受診.肝彎曲部から上行結腸にかけての区域性腸炎の診断で抗結核剤投与を行った.1987年6月より,下痢および発熱が出現し再度入院.脾彎曲部を中心とした縦走潰瘍を認めたことより,大腸Crohn病を疑い,栄養療法を施行したところ病状の改善をみた.1988年6月粘血便の再燃を認めたが,栄養療法の強化により改善した.しかし1989年8月にも再燃し,第3回目の入院.大腸鏡でS状結腸を中心に,膿性粘液の分泌による小白斑が付着する浮腫状の粘膜面を認め,改めて潰瘍性大腸炎と診断した.salicylazosulfapyridineおよびprednisoloneの投与を開始したところ緩解に導入され,以後再燃は認めていない.
A 36-year-old female was admitted to our hospital because of lower abdominal pain and diarrhea in July 1975. Barium enema study revealed segmental colitis at the hepatic flexure. Mucoid diarrhea and high fever developed in June 1987. Barium enema and colonoscopic examinations showed multiple longitudinal ulcers around the splenic flexure and uneven inflammation in the colon, leading to the diagnosis of probable Crohn's disease. In September 1989, however, ulcerative colitis seemed more likely because of the colonoscopic findings, i.e., granular mucosal pattern with shallow ulcerations and diffuse inflammation from the rectum to the descending colon. It is difficult to differentiate ulcerative colitis from Crohn's disease in certain group of patients since clinical features of these diseases overlap each other. Long term follow-up is necessary to make an accurate diagnosis in these cases.
Copyright © 1990, Igaku-Shoin Ltd. All rights reserved.


