Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
患 者:森○運○助 72歳 男
昭和45年8月,疝痛発作あり,救急病院に入院し,総胆管結石の診断にて手術を施行された.しかし,術後も時に38℃~39℃の発熱があり本院に紹介される.
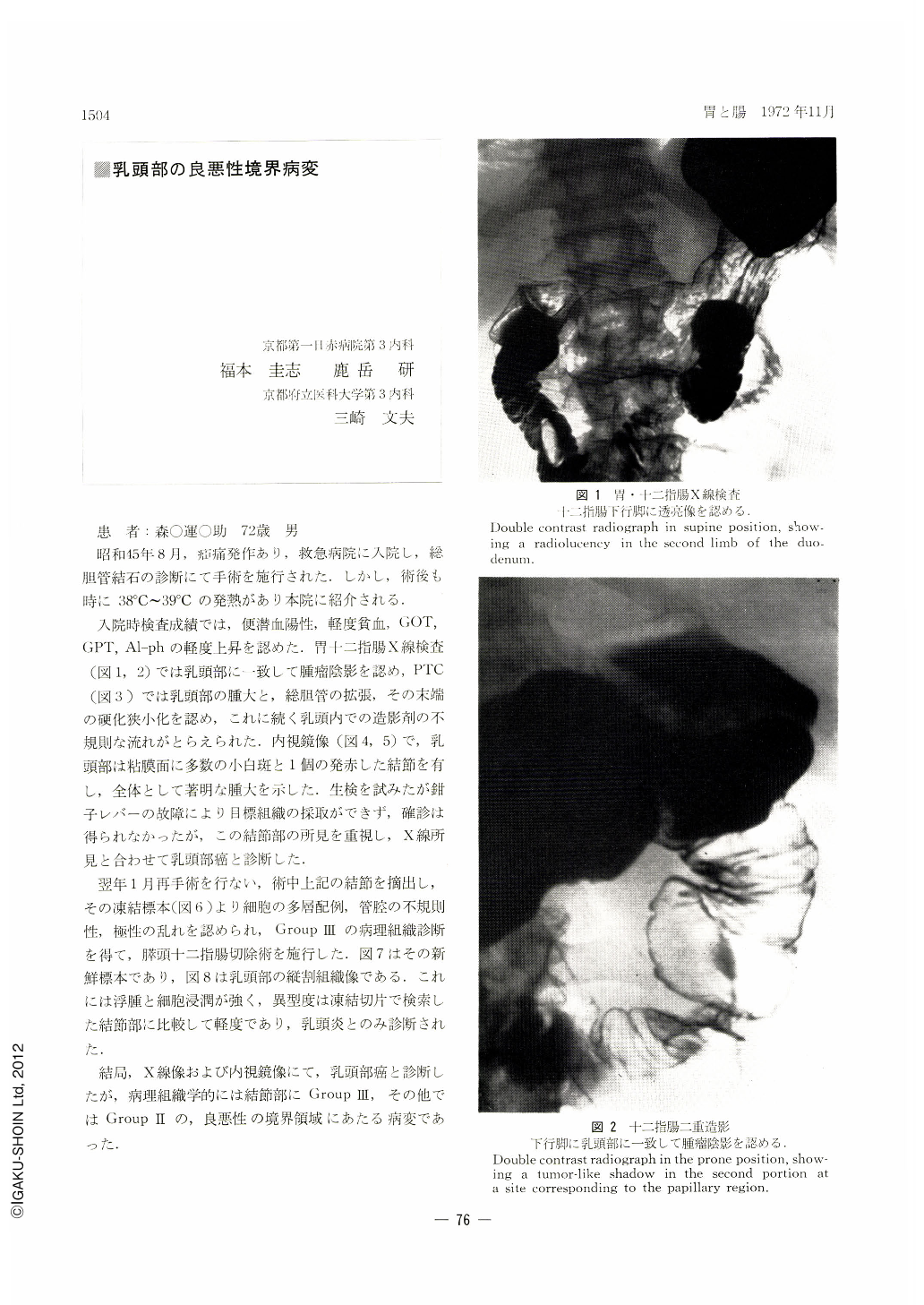
入院時検査成績では,便潜血陽性,軽度貧血,GOT,GPT,Al-phの軽度上昇を認めた.胃十二指腸X線検査(図1,2)では乳頭部に一致して腫瘤陰影を認め,PTC(図3)では乳頭部の腫大と,総胆管の拡張,その末端の硬化狭小化を認め,これに続く乳頭内での造影剤の不規則な流れがとらえられた.内視鏡像(図4,5)で,乳頭部は粘膜面に多数の小白斑と1個の発赤した結節を有し,全体として著明な腫大を示した.生検を試みたが鉗子レバーの故障により目標組織の採取ができず,確診は得られなかったが,この結節部の所見を重視し,X線所見と合わせて乳頭部癌と診断した.
The patient : U. M., a 72-year-old man.
In August 1970 he was admitted to an emergency hospital because he had a bout of colic in the abdomen. He underwent surgical intervention there under a diagnosis of choledocholithiasis. However, even after the operation the fever persisted ranging from 38°to 39℃, so that he was referred to our hospital.
At admission, he was slightly anemic with the stool positive for occult blood. Slight increase was noted in the SGOT, SGPT and alkaline phosphatase. X-ray examination of the upper digestive tract (Figs. 1 and 2) showed a tumor-like shadow at a site corresponding to the papillary region. Percutaneous transhepatic cholangiography (Fig. 3) disclosed swollen papillar region with dilated common bile duct. The distal end of the duct appeared rigid and narrowed, and in the adjacent papilla was an irregular flow of contrast medium visualized. Endoscopic pictures (Figs. 4 and 5) revealed the papillar region having on the mucosal surface a number of tiny white flecks and a reddened nodular lesion. The papillary region was greatly swollen as a whole. Biopsy was tried with little sucoess because the lever in the forceps was out of order and we were unable to obtain specimens from the tissue initially aimed at. It was impossible then to diagnose this case accurrately, but great importance was attached to the findings of the nodule, and, fortified by those of the x-ray, we tentatively diagnosed it as cancer in the papillary region.
The patient underwent re-operation in January of the following year. During the operation the aforementioned nodule was resected, its frozen section (Fig. 6) revealing stratified arrangement of cells and irregular polarity of the glandular structure. Histological diagnosis was made as Grop Ⅲ. Pancreatoduodenectomy was accordingly performed. Figure 7 shows its fresh specimed, and Figure 8 represents histological picture of a longitudinal section of the papillary region. Edema and cellular infiltration are manifest, but its atypicaliry is slighter as compared with the frozen section. Only a diagnosis of papillitis could be made.
The present case seems to exemplify a borderline lesion between malignancy and benignity because diagnosis by both x-ray and endoscopy was cancer of the papillary region and histologically the nodular lesion was confirmed as Group Ⅲ and the other parts as Group Ⅱ.
Copyright © 1972, Igaku-Shoin Ltd. All rights reserved.


