Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
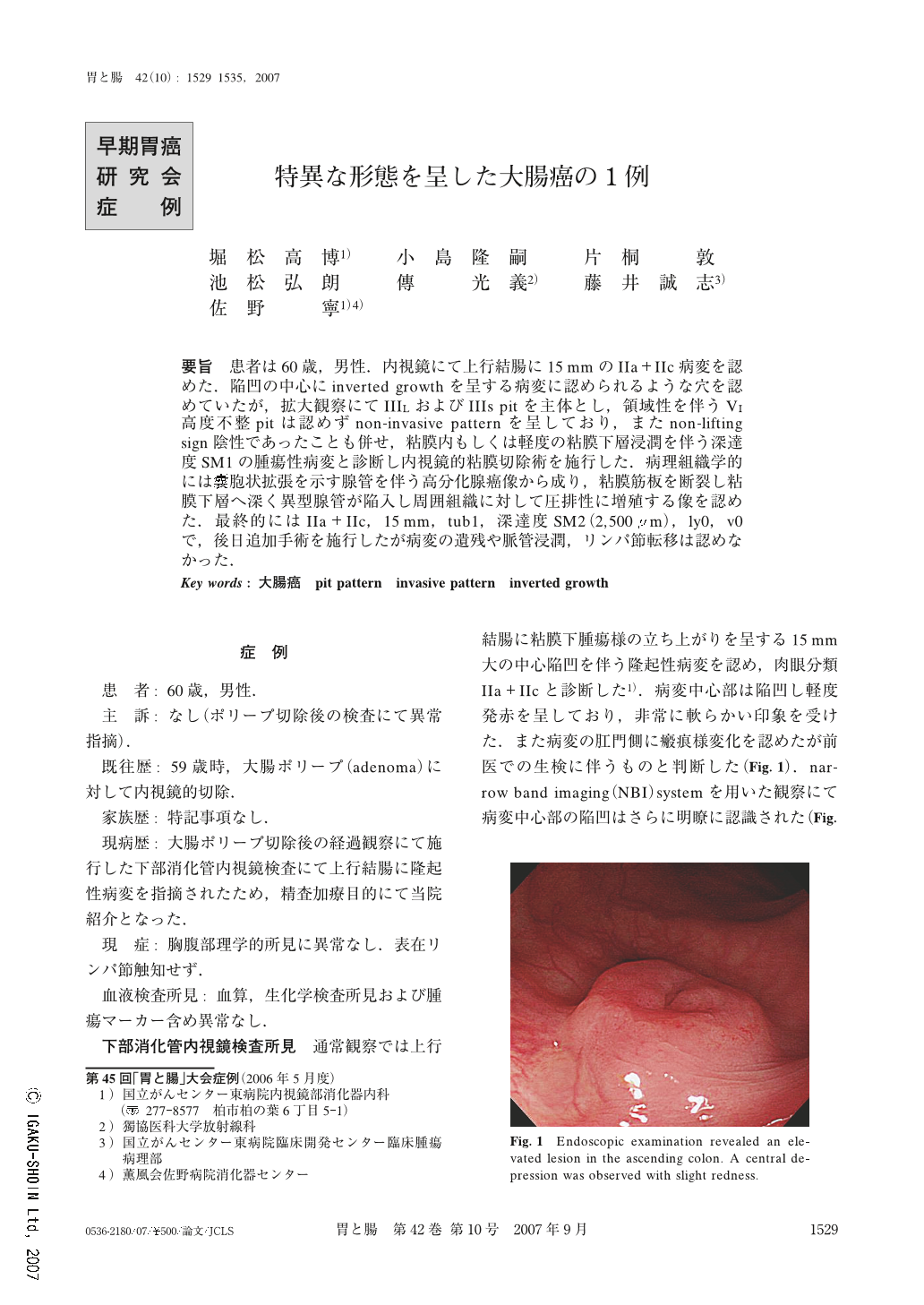
要旨 患者は60歳,男性.内視鏡にて上行結腸に15mmのIIa+IIc病変を認めた.陥凹の中心にinverted growthを呈する病変に認められるような穴を認めていたが,拡大観察にてIIILおよびIIIs pitを主体とし,領域性を伴うVI高度不整pitは認めずnon-invasive patternを呈しており,またnon-lifting sign陰性であったことも併せ,粘膜内もしくは軽度の粘膜下層浸潤を伴う深達度SM1の腫瘍性病変と診断し内視鏡的粘膜切除術を施行した.病理組織学的には嚢胞状拡張を示す腺管を伴う高分化腺癌像から成り,粘膜筋板を断裂し粘膜下層へ深く異型腺管が陥入し周囲組織に対して圧排性に増殖する像を認めた.最終的にはIIa+IIc,15mm,tub1,深達度SM2(2,500μm),ly0,v0で,後日追加手術を施行したが病変の遺残や脈管浸潤,リンパ節転移は認めなかった.
The patient was a 60-year-old male. Endoscopic findings showed a Type IIa+IIc lesion measuring 15 mm in the ascending colon. The hole at the center of the depression area was similar to an inverted hyperplastic polyp, but magnifying colonoscopy showed mainly Type IIIL, IIIs pit pattern and highly irregular VI pit pattern whose demarcated area was not detected, so we defined it as a non-invasive pattern, and diagnosed it as a lesion limited to the submucosal and slightly invasive (below 1,000μm). We performed endoscopic mucosal resection. Histological examination of the resected specimens showed a well-differentiated adenocarcinoma with a gland showing bouton-like expansion, and confirmed that the invasion depth extended to the submucosal layer. Finally pathological diagnosis showed Type IIa+IIc, 15 mm, tub1, SM2 (2,500μm), ly0, v0. Later we carried out a hemi-colectomy, but neither residual tumor nor lymph node metastasis was observed.
Copyright © 2007, Igaku-Shoin Ltd. All rights reserved.


