Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- 参考文献 Reference
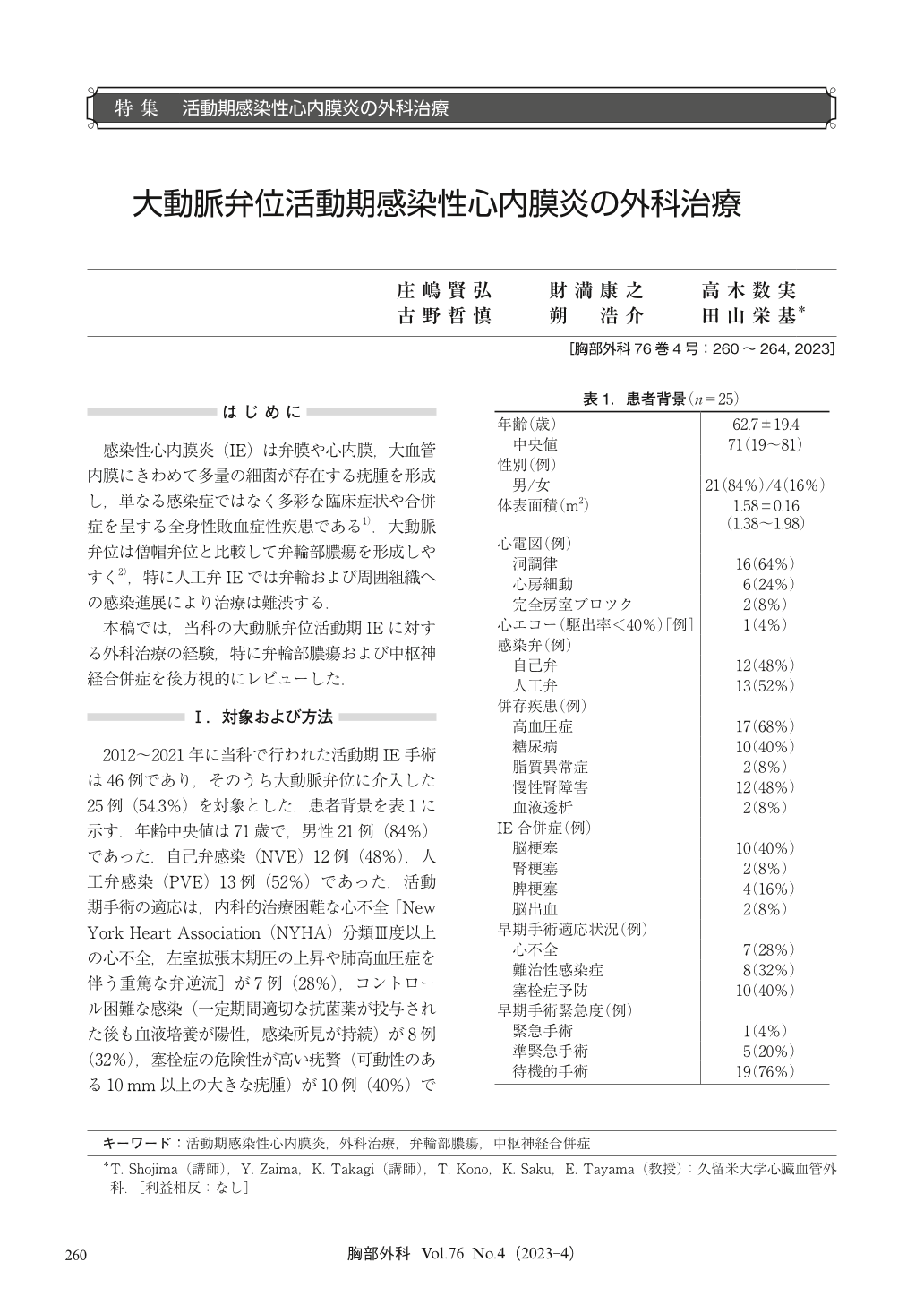
感染性心内膜炎(IE)は弁膜や心内膜,大血管内膜にきわめて多量の細菌が存在する疣腫を形成し,単なる感染症ではなく多彩な臨床症状や合併症を呈する全身性敗血症性疾患である1).大動脈弁位は僧帽弁位と比較して弁輪部膿瘍を形成しやすく2),特に人工弁IEでは弁輪および周囲組織への感染進展により治療は難渋する.
Herein, we retrospectively review our experience with surgical treatment of active aortic valve infective endocarditis, particularly aortic annular abscess, and central nervous system complications. From 2012 to 2021, 46 consecutive patients underwent surgery during the active phase of infective endocarditis, 25 of which were performed at the aortic position. One patient died early (<30 days) due to low output syndrome and another 2 patients who were never discharged died because of general prostration. The actuarial survival rate was 84% at 1 year, and 80% at 3 and 5 years. Eleven patients [6 native valve endocarditis (NVE), 5 prosthetic valve endocarditis (PVE)] had valve annular abscess requiring removal of the infected tissue and reconstruction of a definite anatomic continuity, and aortic valve replacement was subsequently performed in 7 patients and aortic root replacement in 4 patients. Direct closure was performed in 4 patients with partial annulus defects, and reconstruction with an autologous nor bovine pericardium patch was performed in 6 patients with large annulus defects. Preoperative imaging revealed acute cerebral embolism in 10 patients. In eight cases, surgery was performed within 7 days after diagnosis of cerebral embolism. No patient had abnormal postoperative neurological findings. There were no reoperations and no recurrence of infective endocarditis.
© Nankodo Co., Ltd., 2023


