Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
いとぐち
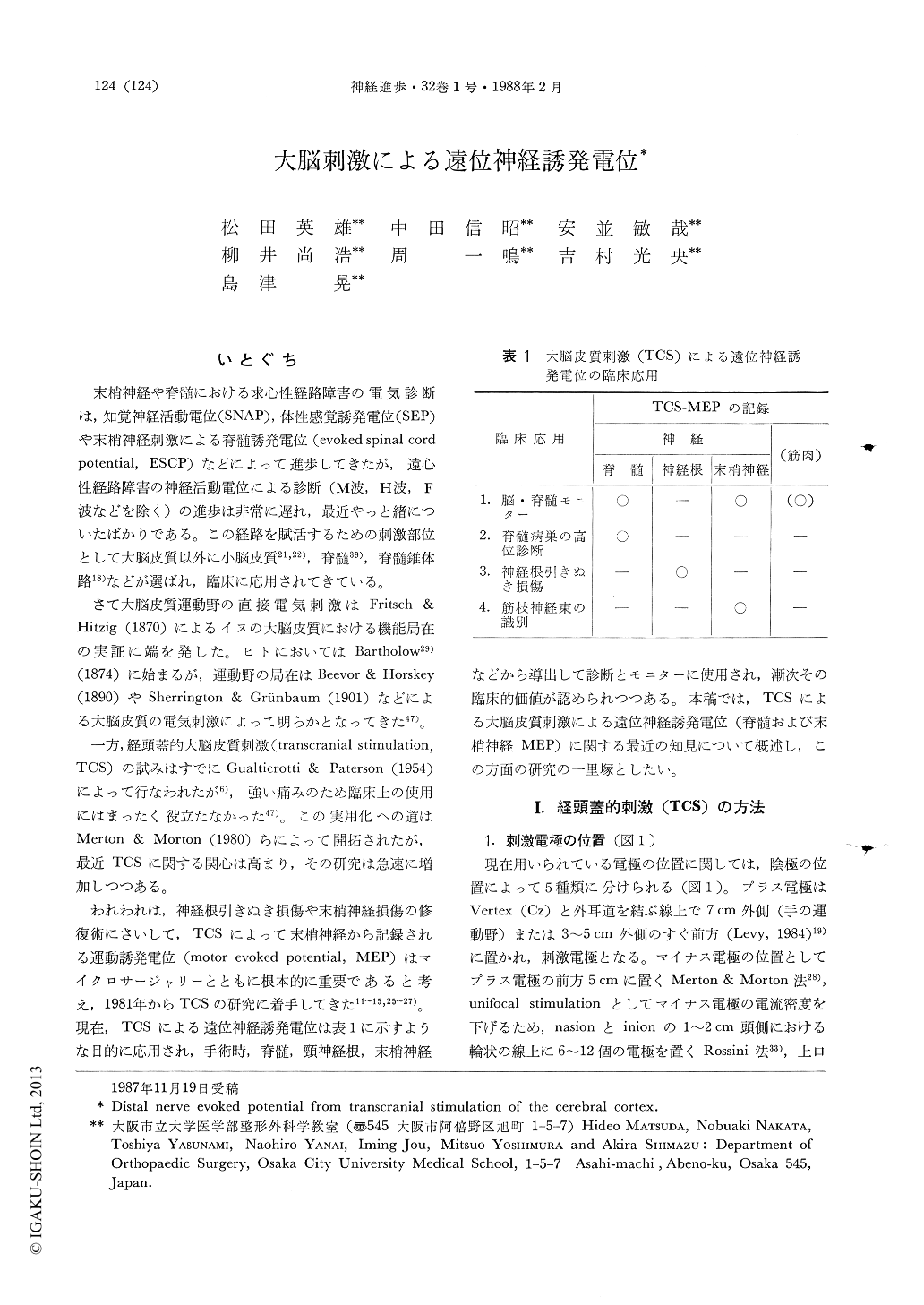
末梢神経や脊髄における求心性経路障害の電気診断は,知覚神経活動電位(SNAP),体性感覚誘発電位(SEP)や末梢神経刺激による脊髄誘発電位(evoked spinal cord potential,ESCP)などによって進歩してきたが,遠心性経路障害の神経活動電位による診断(M波,H波,F波などを除く)の進歩は非常に遅れ,最近やっと緒についたばかりである。この経路を賦活するための刺激部位として大脳皮質以外に小脳皮質21,22),脊髄39),脊髄錐体路18)などが選ばれ,臨床に応用されてきている。
さて大脳皮質運動野の直接電気刺激はFritsch & Hitzig(1870)によるイヌの大脳皮質における機能局在の実証に端を発した。ヒトにおいてはBartholow29)(1874)に始まるが,運動野の局在はBeevor & Horskey(1890)やSherrington & Grünbaum(1901)などにょる大脳皮質の電気刺激によって明らかとなってきた47)。
The usefulness of clinical application of spinal motor evoked potential (MEP) and peripheral nerve MEP elicited by transcranial stimulation (TCS) of the cerebral cortex was described in reference especially to the safety of the procedure. Postoperative motor and sensory disturbances can now be prevented or reduced greatly by evaluating spinal MEP together with spinal somatosensory evoked potential (spinal SEP) during surgery. Spinal MEPs consist of fast and large spike potentials and slow potentials, the occurence of which is not consistent. MEPs are affected by anesthesia, but this tendency is more notable in the latter. For this reason, simultaneous recording above and below the lesion is necessary for spinal monitoring using to sinal MEP as the index. The percent accuracy of the diagnoses in 25 patients with compressive myelopathy and 12 patients with spinal cord tumor was 91.9% according to spinal MEP and 86.5% according to spinal SEP from cauda equina stimulation.
Copyright © 1988, Igaku-Shoin Ltd. All rights reserved.


