Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
- サイト内被引用 Cited by
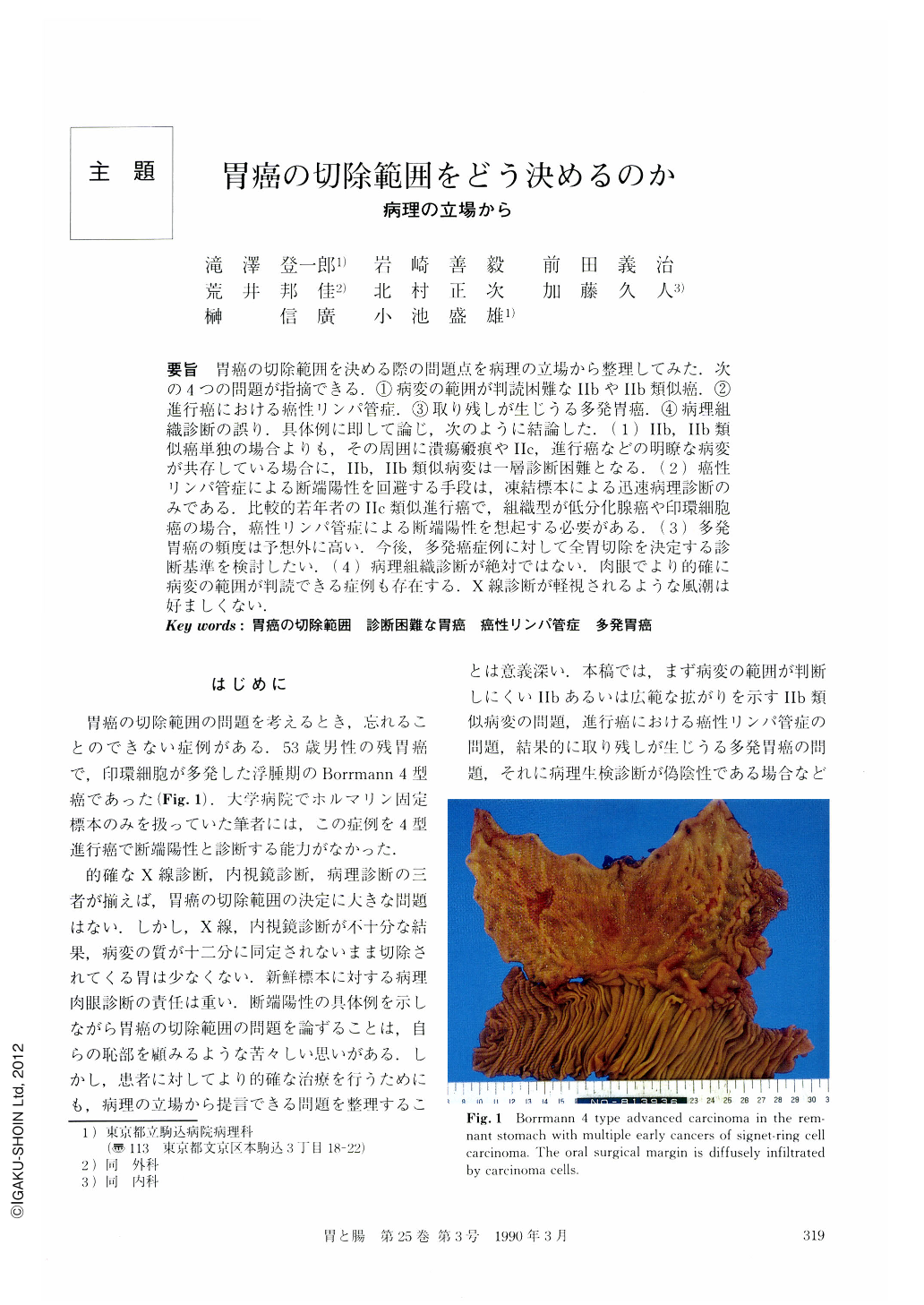
要旨 胃癌の切除範囲を決める際の問題点を病理の立場から整理してみた.次の4つの問題が指摘できる.①病変の範囲が判読困難なⅡbやⅡb類似癌.②進行癌における癌性リンパ管症.③取り残しが生じうる多発胃癌.④病理組織診断の誤り.具体例に即して論じ,次のように結論した.(1) Ⅱb,Ⅱb類似癌単独の場合よりも,その周囲に潰瘍瘢痕やⅡc,進行癌などの明瞭な病変が共存している場合に,Ⅱb,Ⅱb類似病変は一層診断困難となる.(2) 癌性リンパ管症による断端陽性を回避する手段は,凍結標本による迅速病理診断のみである.比較的若年者のⅡc類似進行癌で,組織型が低分化腺癌や印環細胞癌の場合,癌性リンパ管症による断端陽性を想起する必要がある.(3) 多発胃癌の頻度は予想外に高い.今後,多発癌症例に対して全胃切除を決定する診断基準を検討したい.(4) 病理組織診断が絶対ではない.肉眼でより的確に病変の範囲が判読できる症例も存在する.X線診断が軽視されるような風潮は好ましくない.
Exact radiological and endoscopic diagnosis of the cancerous lesion supported by accurate pathologic diagnosis is adequate for precise determination of resection-line in operations for gastric cancer. However, the area of gastric cancer is sometimes inaccurately diagnosed by endoscopic and / or radiological examinations. Macroscopic examination of the surgically resected fresh stomach by pathologists is very important and may be the last chance to correct the misdiagnosis. To determine the precise resection-line, we discuss four pathologic problems; 1) Ⅱb or Ⅱb-like cancerous lesions, 2) lymphangiosis carcinomatosa in advanced gastric cancers, 3) multiple gastric cancers, and 4) miscellaneous problems including misdiagnosis of biopsy-specimen by pathologist, etc.
Conclusions are itemized as follows:
1) For endoscopist, radiologist and pathologist, it is very difficult to judge the boundary of Ⅱb of Ⅱb-like gastric cancer. It seems that it becomes more difficult to judge the boundary in cases in which Ⅱb or Ⅱb-like lesions coexists with other lesions, for example, ulcer scar, Ⅱc or advanced cancer, because such lesions are identified more easily, and then Ⅱb or Ⅱb-like lesion becomes more difficult to detect. Careful endoscopic and / or radiological examination of the gastric mucosa around an easily detectable lesion is very important for the precise determination of the resection-line.
2) The histological characteristics of "crawling cancer" are described, which shows wide intramucosal spreading with Ⅱb-like gross features. When a pathologist notices characteristic features of crawling cancer in biopsy-specimens, it is necessary to discuss the area of the cancer with endoscopists and radiologists.
3) Lymphangiosis carcinomatosa is one of the major problems for precise determination of gastric resection-line, especially in cases of advanced gastric cancers. Frequency of lymphangiosis carcinomatosa in gastric cancers of Borrmann 4 and 3 type is approximately 30%. By naked-eye observation, it is impossible to detect the condition of lymphangiosis carcinomatosa. To make a surgical margin free from cancerous infiltration, microscopic examination of the surgical margin by frozen section is a means which pathologists can use.
4) Ⅱc-like advanced gastric cancer may be accompanied by lymphangiosis carcinomatosa. In some cases of Ⅱc-like advanced cancer in young patients up to the age of sixth, and also in cases of poorly differentiated adenocarcinoma or signet-ring cell carcinoma, microscopic examination by frozen section may be necessary for curative resection of the cancer.
5) In cases with lymphangiosis carcinomatosa extending beyond the line 1 cm beyond the surgical margin, even if the pathologist reports that the margin is free from cancer, it should be considered that the surgical margin is infiltrated by cancer, and close follow-up observations are necessary.
6) In cases of multiple gastric cancers, undetectable cancerous lesions may be left behind in the remnant stomach. Surgically resected stomachs with multiple cancers are very frequent in Komagome Hospital; 25% in the last two years. In cases of multiple gastric cancers, 54.6% of them are advanced cancers with early cancer, and 44.3% are multiple early cancers. More than 90% of the cases with multiple early cancers are composed only of well differentiated tubular adenocarcinoma. As a background of multiple early tubular adenocarcinoma, we observe characteristic atrophic gastric mucosa. By clarification of the pathohistologic and endoscopic features of this background mucosa, it may be possible to identify a high-risk group for tubular adenocarcinoma. Anyway, frequency of multiple gastric cancers is very high, and then partial resection may be insufficient for curative treatment. In the near future, we should make criteria indicating the need for total resection of the stomach in cases with multiple cancers. Our impression is that, in a case with more than four cancers, total resection of the stomach may be necessary, even if partial resection is allowed.
7) Recently, for clinical diagnosis of gastric cancer, endoscopic examination has advantage over radiological examination. Radiological diagnosis may be given little attention. However, in many cases, radiological examination may be more useful than endoscopic examination for correct diagnosis of a cancerous lesion. To determine the precise resection-line, both radiological and endoscopic examinations supported by exact pathologic diagnosis are requisite.
Copyright © 1990, Igaku-Shoin Ltd. All rights reserved.


