Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
I.はじめに
後大動脈(posterior cerebral artery,以下PCAと略す)のP3 portionに動脈瘤の発生する頻度は脳動脈瘤全体の0.3%であり,椎骨脳底動脈系の動脈瘤のうちでも3.1%と比較的まれな動脈瘤である17).この部の動脈瘤に対する手術到達法についてはこれまで十分には検討されていない.今回,くも膜下出血(SAH)にて発症し,subtemporal approachでは到達できなかった後大脳動脈P3 portion動脈瘤の1例を経験した.残念ながらCushing潰瘍からと思われる多量の消化管出血を術後にきたし,他のアプローチによる再手術の機会は与えられなかったが,今回のわれわれの経験は今後このまれな脳動脈瘤を治療する機会に遭遇する脳神経外科医にとって貴重な資料になると考え,同部位への手術到達法に関する文献的知見および考察を加えて報告する.
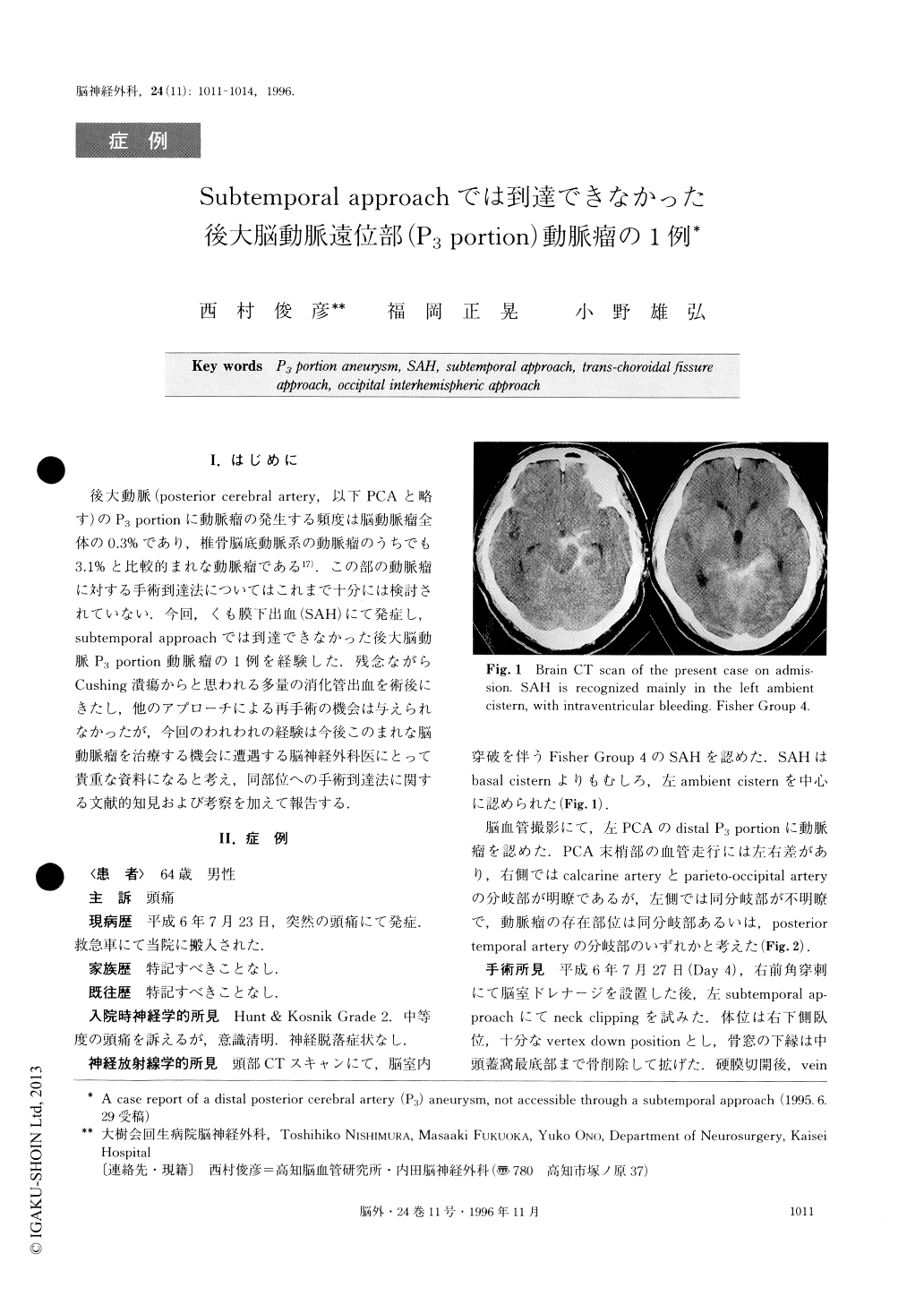
A case of a ruptured aneurysm located in the P3 por-tion of the posterior cerebral artery (PCA), which was not accessible through a subtemporal approach, was re-ported. In addition to the case presented here, alterna-tive operative approaches to the distal P3 portion or higher ambient cistern were reviewed and discussed. A 64-year-old man was admitted because of sudden onset of headache. CT scan disclosed SAH which was recog-nized mainly in the left ambient cistern with in-traventricular bleeding (Fisher Group 4, Hunt and Kos-nik Grade 2). A left vertebral angiogram disclosed a small saccular aneurysm in the distal P3 portion of the left PCA, which was located as highly as the plexal point of the anterior choroidal artery. On day 4, neck clipping was tried via the left subtemporal approach. The distal P3 aneurysm, however, could not be reached by this approach, in spite of aspiration of the parahypo-campal gyrus. On day 7, the patient died of massive bleeding from a Cushing ulcer. It was considered that an occipital interhemispheric approach might have been more suitable in the present case.
Copyright © 1996, Igaku-Shoin Ltd. All rights reserved.


