Japanese
English
- 有料閲覧
- Abstract 文献概要
- 1ページ目 Look Inside
消化管におけるリンパ濾胞増殖について,1941年Marina-Fiol,RofおよびStrömbeckは,回腸終末部のリンパ濾胞とパイエルリンパ濾胞板の増殖例を報告し,1945年にはGoldenがリンパ濾胞増殖症を局所性回腸炎や腸結核と異なった疾患としてNonsclerosing Ileitisと呼ぶことを提唱した.以来,本邦でも白壁,市川らをはじめとする報告が見られるようになった.
また,低ガンマグロブリン血症に伴う下痢症のが注目されていたが,1966年Hermansらが小腸全体のリンパ濾胞増殖症と低ガンマグロブリン血症の合併例を報告し,病態生理学的意義が注目されはじめた.
しかし,大腸におけるリンパ濾胞増殖症に関する報告は少なく,そのほとんどが小児例である.われわれは成人例を経験し,また免疫面も追及しえたので報告する.
Disorders of the nodular lymphoid hyperplasia of the intestine are divided into three groups; lymphoid hyperplasia of the terminal ileum, nodular lymphoid hyperplasia of the small intestine with dysgammaglobulinaemia and lymphoid hyperplasia of the colon. Lymphoid hyperplasia of the colon has been encountered in infants and children and it has been rarely reported in adults. We have recently had an opportunity to study an additional adult case of this disease without immunological abnormality.
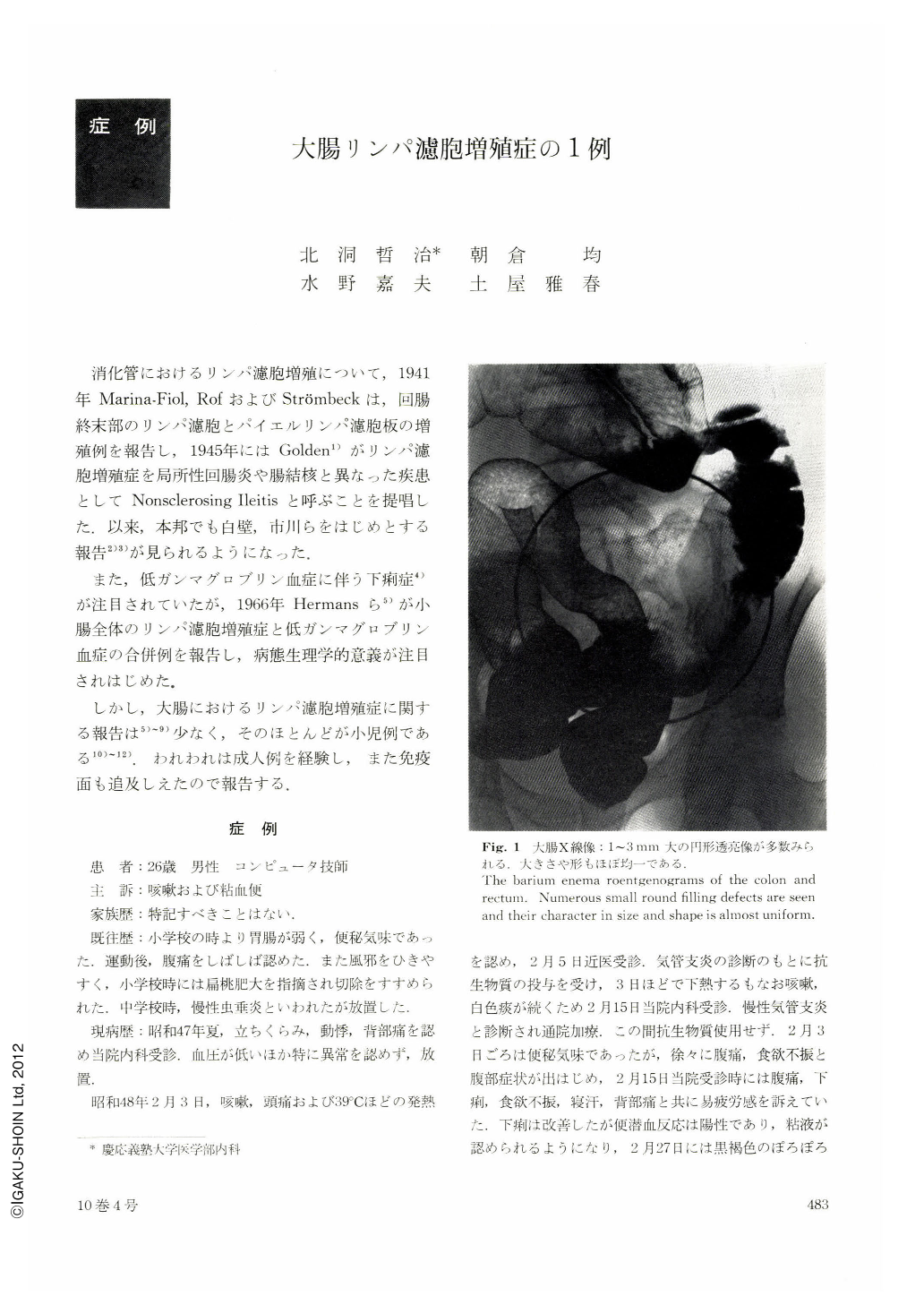
A 26-year-old man was admitted to Keio University Hospital in April 1973 with chief complaints of cough and bloody mucous stools. About two months prior to admission, he had been treated for bronchitis because of cough and fever. Subsequently he complained of abdominal pain, diarrhea, loss of appetite and bloody mucous stools. The cultures of rectal swabs were negative for Shigella dysentery and Salmonella typhi. An air contrast study of the colon showed numerous filling defects 1 to 3 mm in diameter scattered diffusely throughout the colon. Colonofiberscopy revealed numerous small, pale yellow elevated lesions with red halos. Intestinal biopsy specimens obtained from these lesions demonstrated enlarged lymphoid follicles in the mucosa. The physical examination was unremarkable except abdominal tenderness. Laboratory findings were as follows: Examination of stool specimens showed positive occult blood and no Giardia lamblia. RBC was 4.84×106/cu.mm, WBC 6,200/cu. mm, with normal differentials ; serum GOT 57 u, GPT 30 u, Alphosphatase 6.5 u (K. A. units); Serum total proteins 6.6 g/100 ml, and serum protein electrophoresis showed no hypo-γ-globulinaemia. IgG was 1,460 mg/100 ml; IgA 270; IgM 170. Glucose tolerance test was normal. Antinuclear antibody (-), anti DNA antibody (-) populations of T-cell of peripheral lymphocytes was 12% (control: 12±5%), blast transformation of lymphocytes induced by PHA was 62% (control; 50~90%) ; Pneumomediastinography showed no thymic shadow. DNCB skin reactions and PPDS reactions were positive. His condition was improved with treatment of Hypirin and nonspecific drugs. Barium enema and colonofiberscopic examination revealed a normal appearance of the colonic mucosa except in the transverse colon about one month after admission.
Copyright © 1975, Igaku-Shoin Ltd. All rights reserved.


